Non-surgical options for management of hip osteoarthritis: An orthopaedic perspective
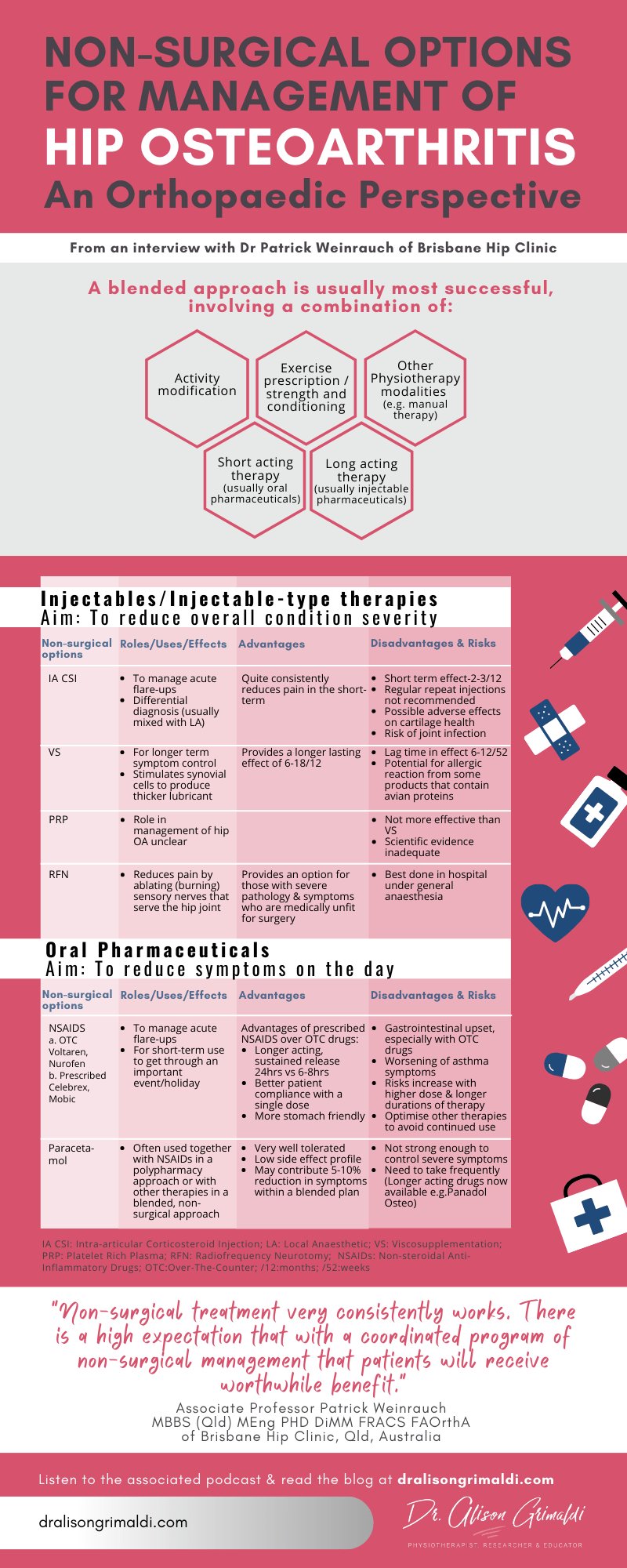
Includes podcast, infographic & podcast notes. Hip Osteoarthritis can be well managed through a blended approach of activity and load modification, exercise therapy and strength and conditioning, manual therapy and a polypharmacy approach of short acting, usually oral pharmaceuticals and long acting, usually injectable pharmaceuticals.
Prior to being considered as a candidate for total hip replacement or resurfacing, most patients with hip osteoarthritis will have undertaken a reasonable trial of non-surgical care. This is because there are many options for non-surgical care that can be blended for successful outcomes for a large proportion of patients until late stage pathology. This podcast will provide a better understanding of a blended approach to non-surgical management of hip OA and the relative indications, risks and benefits of the available pharmaceuticals and injectables.
Listen to the interview here:
About Associate Professor Patrick Weinrauch :
Associate Professor Patrick Weinrauch is an Orthopaedic Surgeon, founder of Brisbane Hip Clinic in Queensland, Australia. The name of his clinic says it all. He focuses exclusively on the management of hip joint disorders, with a high level of experience and expertise in a full range of surgical procedures for the hip, including hip joint arthroscopy, hip joint preservation surgery, hip resurfacing and hip replacement procedures. Dr Weinrauch is a Fellow of the Royal Australasian College of Surgeons and a Fellow of the Australian Orthopaedic Association, and not only has a busy clinical practice but contributes to education programs for other surgeons and health professionals and to scientific research in this field. Dr Weinrauch has published over 50 peer-reviewed scientific papers and is the Deputy Editor for the International Journal of Advanced Joint Reconstruction. He is currently appointed as an Associate Professor at the Griffith University School of Medicine and has been awarded a Doctorate of Philosophy and Master of Engineering for his research relating to the surgical management of adult hip joint disorders. We are very grateful to Patrick for sharing his valuable time and wisdom.
Podcast Notes
Key Point:
Non-surgical treatment very consistently works. There is a high expectation that with a coordinated program of non-surgical management that patients will often receive worthwhile benefit.
The degree of benefit may be variable, determined by:
1. limitations on what we can provide to patients due to their particular circumstances, for example their tolerance/suitability for certain medications
2. degree of wear & dysfunction – with more severe presentations, symptoms may be reduced but the outcomes may still not achieve adequate patient satisfaction
A blended approach to non-surgical management of Hip OA is usually most successful, involving the use of a number of strategies, in combination.
1. Activity modification
2. Exercise prescription/strength & conditioning
3. Other Physiotherapy modalities e.g. manual therapy
4. Long acting therapy – usually injectable
5. Short acting therapy for intermittent flares of symptoms – pharmaceutical tablets
Injectables
The role of injectable therapies is to reduce the overall symptoms – patients will still have symptoms and intermittent flares but the overall severity of symptoms will be reduced.
Types of injections:
1. Intra-articular corticosteroid injection
• Provides quite a consistent positive response but should be used sparingly
• Has limitations
i. Relatively short-lasting effect – 2-3 months
ii. Repeated CSI’s are not recommended as a longer-term strategy
• Best used for
i. Acute exacerbations e.g. for a patient who has been managing well for a long time then presents with an acute, severe flare-up and symptoms need to be settled quickly.
ii. Differential diagnosis e.g. for patients with both lumbar and hip pathology, an intraarticular hip CSI may help clarify the relative contribution of the hip to current symptoms. In this situation the steroid would usually be mixed with a local anaesthetic, for a combined diagnostic and therapeutic effect
• Risks/Contraindications
i. There is concern that corticosteroid may be detrimental to chondral health and may accelerate the degree of degenerative change
ii. Also risk of introducing infection into the joint, with any intra-articular injection. These risks are low but with higher frequency of injection comes higher risks.
2. Viscosupplementation
• Provides a longer lasting effect – variable but usually 6-18 months
• Modest effect on symptoms – commonly 30-40% reduction
• Types of pharmaceuticals used for Viscosupplementation: Durolane, Euflexxa, Synvisc
• Procedure performed in clinic, under ultrasound guidance
• Absorbed by the synovial lining of the hip joint, which produces the lubricant (synovial fluid) for the hip joint. The pharmaceutical stimulates the synovial cells to produce thicker lubricant, increasing viscosity of the synovial fluid within the joint.
• Effect is limited to the joint that is injected
• Lag time in effect while the biological response develops
i. 50% of effect by 6 weeks
ii. Maximal effect by 3 months
• Frequency of repeat injections: Shortest timeframe for repeat injection would usually be 6 months. If symptoms are not improved for at least 6 months, persisting with repeat viscosupplementation injections is unlikely to be successful.
• Risks/Contraindications
i. Allergy – some products contain avian proteins – not suitable for those with allergy to chicken or egg. There are pharmaceuticals available without avian proteins, so selection of the particular pharmaceutical will avoid problems.
3. Platelet Rich Plasma
• Role in management of hip OA unclear at present
• Scientific evidence for PRP for hip OA is inadequate
• Not been shown to be more effective than viscosupplementation
4. Radiofrequency ablation/neurotomy (injection-like therapy)
• Relatively new procedure around the hip
• Involves placing needle with electrified tip close to hip joint at specific locations, to ablate small sensory nerves that serve the hip joint
• Not possible to access all sensory nerves that serve the hip joint, so the procedure will reduce but not remove all sensation from the hip joint
• When used together with viscosupplementation, see longer lasting effects in terms of symptom reduction
• Best done in a hospital under a general anaesthetic, so therefore more considerations regarding general applicability or ease of this treatment
• Therefore, tends to be used sparingly in specific scenarios, e.g. where a patient has very severe pathology and symptoms but is medically unfit for joint replacement surgery and is not responding to other non-surgical interventions
Oral Pharmaceuticals
The role of oral pharmaceuticals is to provide short acting relief for intermittent symptoms. They allow treatment of the symptoms on the day. If the patient is requiring high doses of oral pharmaceuticals regularly, management of overall symptoms is not optimal and should be reviewed.
1. Non Steroidal Anti-inflammatory Drugs (NSAIDs)
• Best used
i. short term for acute flare ups
ii. to provide a ‘pharmaceutical holiday’ from symptoms, e.g. to get through an important activity or short holiday. May take medications for a couple of days – a couple of weeks.
• Risks - regular ongoing use poses health risks
i. Gastrointestinal upset
ii. Worsening of asthma symptoms in those with asthma
iii. Risk profile increase with dose and duration of therapy
• FALSE – that a patient needs to continue take the medication continuously to get an effect. Instead, dose should be titrated depending on symptoms.
• Types of NSAIDs
i. Over the counter – Voltaren, Nurofen
ii. Prescription NSAID’s (Celebrex, Mobic) do have advantages
1. Longer acting therapies – sustained release, providing an effect over a 24 hour period, as opposed to a 6-8 hour effect from over the counter medications
2. Compliance with dosing is better as the patient only needs to take the medication once/day
3. More ‘stomach-friendly’, less gastrointestinal irritation
2. Paracetamol
• Often used together with NSAIDs in a ‘polypharmacy’ approach
• Very well tolerated for the vast majority of people & very low side effect profile
• Not strong enough to control severe symptoms, but within a blended approach with other non-surgical management strategies, paracetamol use may have some merit, even if only providing a 5-10% reduction in symptoms
• Need to take it quite frequently as most preparations are short acting, but longer-acting paracetamol preparations are now available – Panadol Osteo
Supplements
• Generally safe with a low side-effect profile. Many people have tried at least 1-2 supplements before seeing an orthopaedic specialist
• Most commonly used natural adjuncts are Glucosamine and Fish Oil
• Evidence is weak with any effect likely to be small
That it’s for Part 2 of this interview series. If you are not signed up to the www.dralisongrimaldi.com mailing list, sign up today to ensure you don’t miss the last of this great series, which will be a video interview that explores the different prostheses, surgical approaches and their indications. Don’t forget to explore the dralisongrimaldi.com site where you’ll find a wealth of clinically applicable information on all things hip.
Learn more about
CONTEMPORARY DIAGNOSTIC & MANAGEMENT STRATEGIES FOR ANTERIOR HIP & GROIN PAIN, here
Another great Anterior Hip Pain blog

Anterior Hip Pain: Causes & Contributing Factors
Adequate consideration of individual causes and contributing factors is important for best outcomes.
Discover our Anterior Hip & Groin Pain Course
If you enjoyed this blog, you might like to take the online course on Anterior Hip & Groin Pain - 5 hours of guided online video content. Better your skills and understanding of the anterior hip and groin and become equipped with the knowledge to administer clinical diagnostic tests and management strategies.