Load management is not just doing less

Discover our Lateral Hip & Buttock Pain Course
If you enjoyed this blog, you might like to take the online course on Anterior Hip & Groin Pain - 6 hours of guided online video content. Examine various joint-related, soft tissue-related and nerve-related conditions associated with lateral hip and buttock pain, their mechanisms, associated impairments, clinical diagnostic tests and management approaches. To learn more, take the lateral hip and buttock pain online course, or join me in an online or practical lateral hip and buttock pain workshop.
A ‘load management and exercise’ approach is a central pillar commonly reported to underpin contemporary management of musculoskeletal conditions. However, when we dive into the detail, exercise selection for the same type of presentation or injury is often quite disparate. It is to be expected that there will be appropriate individualisation of an exercise program depending on for example, the patient’s specific impairments, comorbidities, functional requirements and preferences. However, clinician education and clinical beliefs and bias will also play a role. So, what of load management? Do we all speak the same language here? What does this broad term – ‘load management’ actually mean? While there will be differences in opinion on the definition of load management, an important message I wanted to highlight in this blog, is that load management is not just doing less!
Load management is not just doing less physical loading - managing biopsychosocial loads
It is now clear that the pain experience is not simply a response to biological overload of some form. Psychological factors and social circumstance can also burden an individual and influence their pain experience and health status. The relative strength of contribution of biopsychosocial factors will vary between individuals. A comprehensive approach to load management will need to consider all these factors and address dominant factors for the individual - load management is not just doing less physical loading.
In contemporary clinical practice, we are much more aware of the value of identifying and managing psychological contributors, particularly in persistent pain states. There may be fear and distress directly related to nociceptive pain or injury, for example, the patient is concerned about the source of the ‘pain’ (nociception) – ‘maybe I have cancer’ – or distressed about potential consequences of the situation – ‘how will this impact on my work, physical activity, health, family or future?’ The patient’s condition may also be causing sleep disturbance, directly impacting on mental fatigue and distress. Allowing time for, or directly eliciting discussion about these facets of the pain experience may highlight psychological loads that need to be addressed with priority.
At a minimum, providing a thorough assessment and a clear explanation of the presenting condition can be reassuring for the patient – at least this clarifies what ‘it’ is or what ‘it’ is not. A discussion around prognosis can provide realistic expectations and set the framework for development of a collaborative plan to manage and minimize the impact on that individual’s work, physical activity, health, family or future. Assisting with sleep hygiene and providing positioning advice to reduce condition-specific provocation (e.g., compressive loading of the gluteal tendons in sidelying in someone with gluteal tendinopathy), can for some people have a marked impact on recovery rate and overall success of an intervention.
Then of course there are psychological contributors that will impact on a patient’s pain experience that have not developed in response to a musculoskeletal condition – other work or life stressors that put the endocrine, immune and pain system defences on high alert. For some patients, failure to address such stressors will hamper rehabilitation attempts. Most clinicians working in musculoskeletal rehabilitation will be able to provide some basic advice and direction for self-management of psychological distress but will not usually be adequately skilled to provide comprehensive psychological interventions. The role here will be to identify such situations, thoughtfully explain the relationship between psychological stressors and pain and discuss involvement of another health professional within the overall management plan.
Load management - reducing overall exposure
Let’s return now to discussing biological overload and load management strategies. It has been my experience as an educator, mentor and researcher, that many clinicians interpret load management to mean simply doing less. The patient reports that it hurts to run, the therapist advises the patient to stop or reduce running for a period of time and then gradually build up again.
Controlling overall exposure to load is certainly a key principle of load management and will be particularly pertinent where pain onset or injury has occurred subsequent to a rapid increase in volume of athletic training or physical activity.
Common examples of training volume overload:
- Starting an unaccustomed activity
- signing up for boot camp (high intensity group training)
- starting at the gym
- starting a Couch to 5k running program
- joining a walking or running group
- going on an active holiday when activity levels are generally low
- Returning to full training load too quickly after illness or injury
- Spiking training too rapidly due to an upcoming event, competition or the start of a sporting season.
Too much, too little or both – acute and chronic workloads
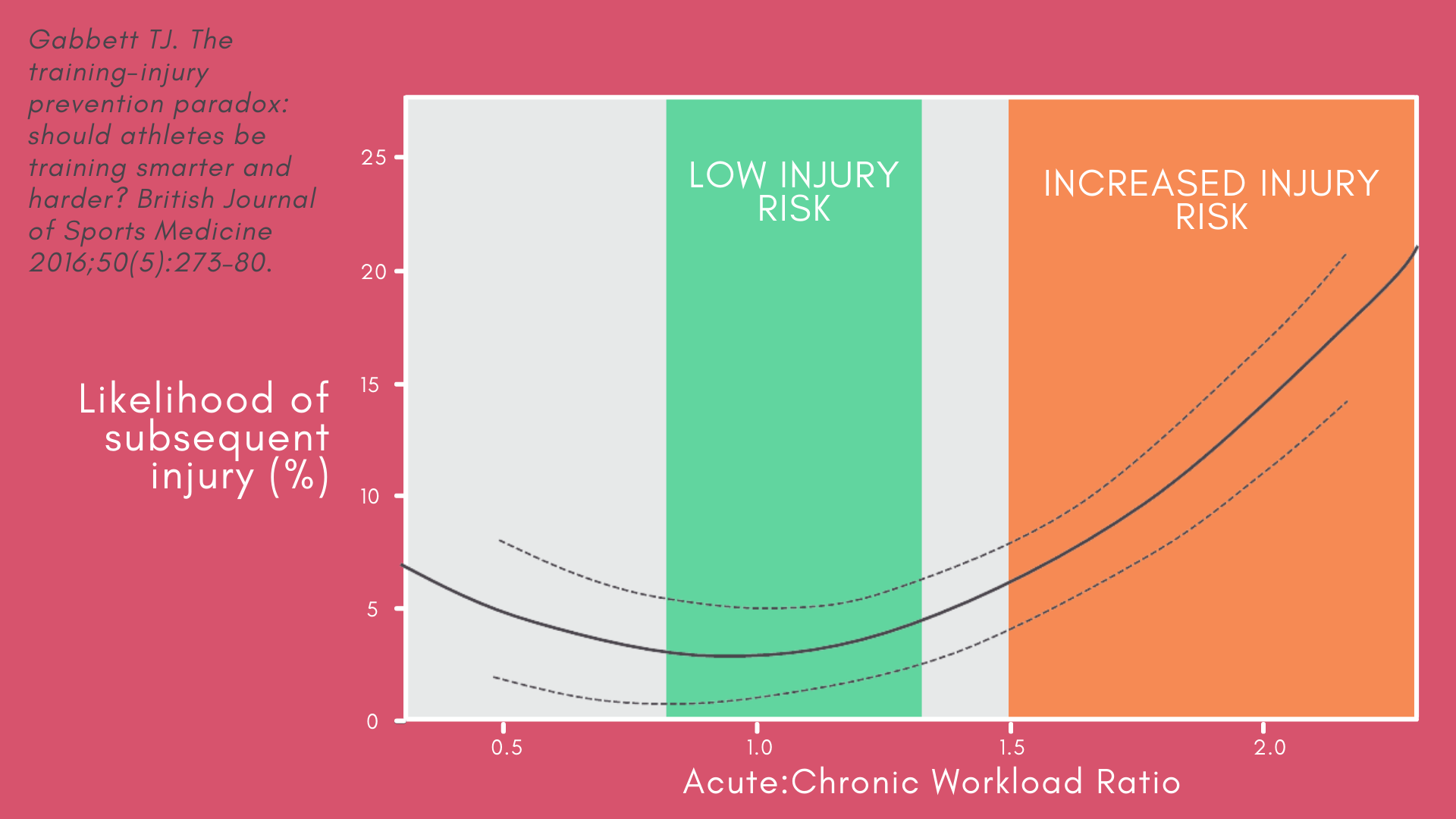
We often see a peak in presentation of patients with overload conditions in the new year, secondary to new year’s resolutions or in preseason periods where the acute:chronic workload ratio has escalated into a high injury risk zone.1 While ‘relative rest’ may be warranted in early phases of rehabilitation of acute and severe presentations, too much rest is likely to put the patient at higher risk due to reduced tissue tolerance, among other factors. Similarly, while allowing adequate time for recovery is important for restoring mechanobiological homeostasis,2 too much recovery time might increase rather than reduce injury risk. Research has demonstrated that low chronic workload and the acute:chronic workload ratio are more predictive of injury than between-match recovery time in Rugby players.1 Acute workload refers to the cumulative training load over the last week, while chronic workload refers to the average workload over the previous 4 weeks. The diagram below from Tim Gabbett’s excellent work on this topic demonstrates that there appears to be a sweet spot in the acute:chronic workload curve, where there is not a large discrepancy in acute versus chronic load and injury risk is lowest.3 However, ratios of 1.5 or greater are considered to put the athlete in a danger zone for injury. The ratio will increase either due to relative increases in acute workload, reductions in chronic workload or both.
Measuring external and internal workload – the usefulness of RPE-Load
In elite sports, measurement of workload often involves use of technology such as GPS trackers and accelerometers. Outside elite sport, such devices may be relevant for some of your more enthusiastic, tech-savvy patients but generally measurement of workload will need to be more low-tech. RPE-Load is a useful way to measure training load that requires no special technology.4,5 RPE-Load is calculated by multiplying the individual’s Rating of Perceived Exertion (RPE) for an exercise or training session by exercise duration. RPE can be measured by using the Borg CR100 scale® where 0 = nothing at all (no exertion at all) and 100 = max (almost maximal exertion). In clinical practice, this is often truncated to a 0-10 scale. The RPE-Load measurement can be then used to calculate acute and chronic (4 weeks of exercise minimum is required) workload and the acute:chronic workload ratio. This metric allows tracking of both external (duration of training) and internal (RPE) loads and is applicable regardless of the sport or activity your patient is undertaking.
Measuring internal load and fatigue of elite athletes often involves monitoring changes in physical performance and/or in cardiorespiratory, blood and saliva markers to track biochemical, hormonal and immunological status. However, subjective measures are often more responsive than objective measures to changes in training load.6 The Profile of Mood States screening tool is commonly used in athletes to gauge internal aspects such as tension, depression, anger, vigour, fatigue and confusion.7 For those less keen to submit to multiple regular questionnaires or physical capacity assessments, the RPE-Load measurement tool is a quick and easy way to track and guide loading for patients with a wide range of physical requirements and goals.
Load management – controlling rate of load increase
Apart from overall volume of loading, indices such as rate of load increase and type of loading may influence pain and injury risk. Rapid change in training load between weeks has been shown to increase injury risk. While up to a 10% increase is usually well tolerated, injury risk in professional athletes has been shown to jump significantly at the 15% mark.3 For those starting from ground zero, for example jogging 100metres, at increases of only 10% per week it will take an extremely long time to reach that 5km target. Novice runners have been shown to tolerate 20-25% increases per week without a substantial increase in injury risk.8 While there is no single rule for all situations, for those who are already active, the 10% per week rule can be a useful general guide for injury prevention and restoring normal training loads after injury. A load monitoring approach - monitoring acute and chronic loads, RPE-Load and changes in symptoms during activity, in the 24hours after and week to week, will assist in determining the appropriateness of the rate of load increase in the context of rehabilitation.
Load management – controlling type of load
The other consideration in a load management program is not just the volume of loading but the type or nature of loading. Different types of musculoskeletal tissues are variably resistant to specific types of load, and rehabilitative programs need to gradually build towards maximal loading scenarios that the individual will be required to tolerate – e.g., high impact for bone, eccentric contractions for muscle (particularly at speed and in a lengthened position) and energy storage and release tasks for tendons (running, jumping, plyometric activity).9
A patient therefore may be able to maintain a reasonable level of activity or loading during rehabilitation by altering load type and ‘relatively resting’ from more demanding tasks for that tissue until tissue capacity can be gradually increased. An activity (load) ladder can be useful for the patient, to guide them on selection of activities appropriate to symptoms. The guide below is not meant to be a definitive guide that will suit all individuals with gluteal tendinopathy, but an example of how you might create an activity ladder for your patient. This guide also does not suggest that everyone must start at the bottom of the ladder - the start point would be different for each individual depending on current capacity and symptoms.

Load management – controlling condition-specific loads
Even with adequate attention to overall load, the rate of load increase and the type of load, some patient’s pain will recur as they are gradually re-exposed to their particular aggravating factors. This can be frustrating for both patient and clinician. The missing piece of the puzzle may well be a lack of attention to condition or region-specific loads incurred during those provocative tasks. In some professional circles there has been a strong shift away from biomechanical or kinematic assessments and interventions. The philosophy appears to be a steadfast but perhaps overly optimistic belief that the human body can adapt to anything, as long as the individual is not fearful of the task. While mindset will have a potent impact on conscious interpretation of sensory stimuli, at a tissue level there is ultimately a limit to adaptive capacity.
Let’s consider a patient with Femoroacetabular Impingement Syndrome (FAIS) associated with a large cam morphology, say an alpha angle of 80° (cam classified in those with angles of 60° more). The patient has presented with flexion-related hip pain, their pain provoked by deep squats and leg press. Do we simply reduce the volume of squats and deadlifts they do for a while, educate them that there is nothing to be feared and then gradually reintroduce them to those same activities? Will that acetabular rim cartilage adapt to the shearing force imposed by the cam morphology in deep flexion? Highly unlikely! Does this mean the patient should avoid the gym and live the rest of their life in fear of flexing their hips? No! But there are some simple strategies that can be employed to better control this condition-specific load. I have talked about such strategies in previous blogs, such as my last blog on modifying leg press for hip pain.
For a patient with gluteal tendinopathy, simply reducing hill walking and stairclimbing and then gradually rebuilding the volume of these tasks may result in unnecessary symptom recurrence. Those with gluteal tendinopathy are more likely to move in ways that overload the abductor tendons.10 Strengthening alone may not alter biomechanics and associated tendon loads. Specific load management advice in the form of simple movement tips or training can be a key element of restoring and maintaining function (and patient confidence) in the short and long term.
Load management is a central element of musculoskeletal rehabilitation, but the scope and wider potential for optimising outcomes through load management is often under-recognised. A simplistic ‘relative rest and reload’ approach may work for some but is often inadequate for recurrent or persistent conditions. Let’s compare a situation of primary biological overload to a primary psychological overload. If a health professional was managing a patient who was not coping psychologically in their work environment, would it make sense to give them time off work and then gradually rebuild their work hours without addressing any of the underlying factors? Success would seem far less likely than an approach that identified and addressed modifiable stressors and built strategies to cope with non-modifiable stressors.
Similarly, in the management of musculoskeletal conditions, load management is not just doing less. Load management must consider biopsychosocial stressors and not simply volume of current loading but chronic workloads, the acute:chronic workload ratio, rate of load increase, as well as tissue-specific and condition-specific loading. Different factors will be variably important for each individual, but a broader awareness of load management principles may assist in expedited and more successful longer-term outcomes.
Another great Lateral Hip Pain blog
Lateral Hip Pain: Causes, Diagnosis, and Treatment
Sign up to my mailing list, and enjoy my monthly Hip Fact files, and lots more exciting behind the scenes content!
References
- Hulin BT, Gabbett TJ, Caputi P et al. Low chronic workload and the acute:chronic workload ratio are more predictive of injury than between-match recovery time: a two-season prospective cohort study in elite rugby league players. Br J Sports Med. 2016;50(16):1008–12.
- Magnusson SP, Langberg H, Kjaer M. The pathogenesis of tendinopathy: balancing the response to loading. Nat Rev Rheumatol. 2010 May;6(5):262-8.
- Gabbett TJ. The training-injury prevention paradox: should athletes be training smarter and harder? Br J Sports Med 2016;50(5):273–80.
- Fanchini M, Ghielmetti R, Coutts AJ et al. Effect of training session intensity distribution on session rating of perceived exertion in soccer players. Int J Sports Physiol Perform 2015;10(4):426–30.
- Napier C, BSc MR, Menon C, Paquette MR. Session rating of perceived exertion combined with training volume for estimating training responses in runners. J Athl Train. 2020;55(12):1285-1291.
- Saw AE, Main LC, Gastin PB. Monitoring the athlete training response: subjective self-reported measures trump commonly used objective measures: a systematic review. Br J Sports Med 2016;50(5):281–91.
- Morgan WP, Brown DR, Raglin JS, O'Connor PJ, Ellickson KA. Psychological monitoring of overtraining and staleness. Br J Sports Med. 1987 Sep;21(3):107-14.
- Nielsen RO, Cederholm P, Buist I et al. Can GPS be used to detect deleterious progression in training volume among runners? J Strength Cond Res 2013;27(6):1471–8.
- Cook JL, Docking SI. "Rehabilitation will increase the 'capacity' of your …insert musculoskeletal tissue here…." Defining 'tissue capacity': a core concept for clinicians. Br J Sports Med. 2015 Dec;49(23):1484-5.
- Allison K, Wrigley TV, Vicenzino B, Bennell KL, Grimaldi A, Hodges PW. Kinematics and kinetics during walking in individuals with gluteal tendinopathy. Clin Biomech (Bristol, Avon). 2016 Feb;32:56-63.