4 of 12 Top Hip Papers of 2024 | Incontinence and complications after hip and knee replacement
Welcome back for day 4 of my 12 Top Hip Papers series of miniblogs from 2024. If you missed Day 3, you'll find a link at the bottom of this page to take you back. The featured paper for day 4 explores incontinence as a risk factor for complications after hip and knee replacement. Read more below with key findings of this paper and the clinical implications.
Discover our Anterior Hip & Groin Pain Course
If you enjoyed this blog, you might like to take the online course on Anterior Hip & Groin Pain - 5 hours of guided online video content. Better your skills and understanding of the anterior hip and groin and become equipped with the knowledge to administer clinical diagnostic tests and management strategies.
4 of 12 Top Hip Papers of 2024: Incontinence is a risk factor for complications after hip and knee replacement1
Background:
- Urinary incontinence has been linked to worse postoperative pain, decreased physical function, and reduced quality of life following total joint arthroplasty.
- Urinary incontinence is also a strong risk factor for urinary tract infection, which may increase the risk of prosthetic joint infection following total joint arthroplasty.
Study Aim:
- To determine whether incontinence is associated with increased postoperative medical and joint complications following primary total hip arthroplasty and total knee arthroplasty.
What was done:
- A retrospective cohort study using a national database of over 600,000 American patients who had undergone hip or knee arthroplasty across the time period 2010 - 2021.
- Patients with incontinence were identified.
- In order to reduce confounding bias, patients with incontinence were matched at a 1:4 ratio with controls, matching for age, sex and a number of other medical factors.
- Rates of medical complications during the hospital stay and within 90 days postoperatively were obtained.
- Joint complications were evaluated at 2 years postoperatively.
- Statistical relationships between urinary incontinence and post operative complications were analysed.
Total Hip Arthroplasty
Patients included:
- 32,811 with incontinence (82% females; mean age 69)
- 129,072 without incontinence (controls) (82% females; mean age 69)

Total Knee Arthroplasty
Patients included:
- 91,935 with incontinence (85% females; mean age 68)
- 367,285 without incontinence (controls) (85% females; mean age 68)
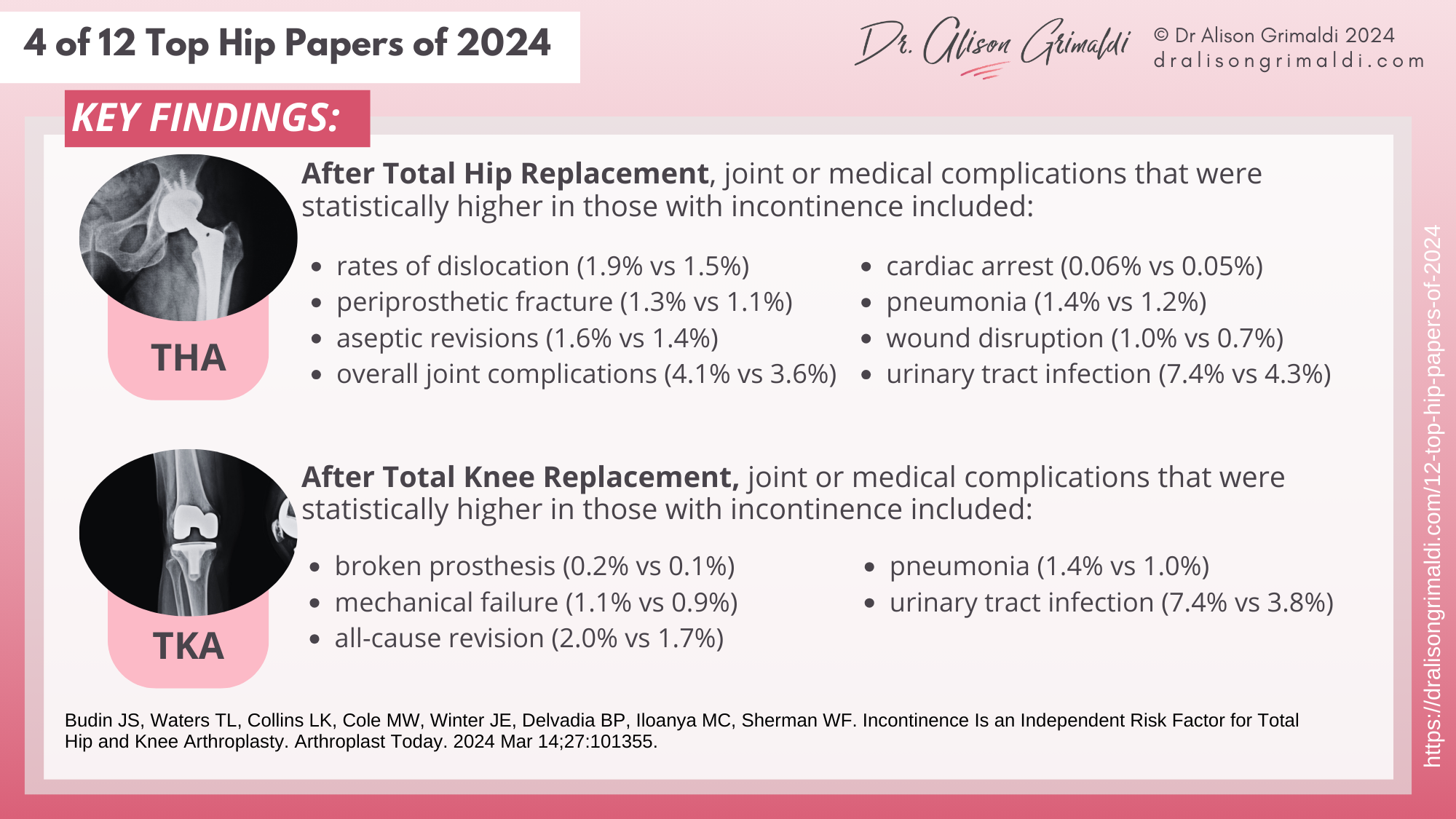
Key Findings:
- Those with urinary incontinence had statistically higher rates of medical and joint complications following total hip arthroplasty and total knee arthroplasty. See the details in the infographic below.
Clinical Implications:
- Incontinence is more common in those with medical conditions such as Multiple Sclerosis and Parkinson’s disease but remains an independent risk factor for both medical and joint complications following total hip and knee replacements.
- Screening for and attending to urinary incontinence before and after total hip and knee arthroplasty may assist in reducing post operative complications.
Those with incontinence had higher risks of joint and medical complications, particularly in females after total hip replacement. While chronic disease status is linked - incontinence is more prevalent is those with Multiple Sclerosis and Parkinson's disease - incontinence remains an independent predictor of increased post-operative complications. Pelvic floor and hip muscle function are both known to be poorer in those with incontinence, and continence and muscle function may both be influenced by hip arthroplasty.
Optimising pelvic floor and hip muscle function pre-operatively may assist in reducing complications after total hip and total knee arthoplasty. Working on continence post-operatively in an holistic approach to rehabilitation may also optimise outcomes and reduce complications. Rehabilitation professionals should screen patients pre and post arthroplasty for continence issues and include attention to continence and the pelvic floor as part of the overall management plan. Co-ordination with a Pelvic Health physiotherapist is likely to produce best results.
Like to learn more about:
- relationships between the hip and pelvic floor?
- optimising pre- and post-operative care for those undergoing total hip arthroplasty?
In Hip Academy, you'll find additional focused videos on both of these topics, as well as downloadable pdf resources.
ALL THIS AND MUCH MORE AT HIP ACADEMY
Join our community of Hip Lovers & Hip Learners at Hip Academy, and experience the confidence that comes with access to high-quality continuing professional development, resources and support.
I hope you enjoyed the infographics and key learnings from Day 4 of my 12 Top Hip Papers of 2024. There are 8 more papers to come in this series, so keep an eye out below as they come out, to see what other top papers and infographics I have prepared for you!

Have you heard about Hip Academy?
Enjoy the benefits of a world class educational Hip Program, specifically designed by Dr Alison Grimaldi to help improve your knowledge surrounding the Hip and Pelvis, and become an expert in your field.
With all Hip Courses included, enjoy all the extra inclusions, including; access to the entire eBook series, growing video library, expanding PDF resource centre, regular member meetings, forums + lots more!