Standing posture, hip joint loads & the management of hip pain
In recent years, particularly in the social media sphere, there has been a lot of negative publicity directed towards management approaches for musculoskeletal pain that address posture and/or incorporate movement training. The criticisms usually hang on two main assertions:
1. Postural and/or movement training will induce hypervigilance and fear avoidant behaviour &
2. That the body is robust and will simply adapt to overcome any loading scenario
I would certainly agree that there are potential adverse effects associated with health and exercise professionals leading people to believe there is only one ‘correct’ posture, or teaching people to consciously maintain some inefficient form of active muscle holding - most commonly an abdominal or gluteal contraction in the context of hip pain presentations. However, we cannot completely ignore the influence of loads encountered during sustained postures or repetitive movements. We are all affected by gravity and how we position our body segments relative to gravitational forces, strongly influences the distribution of loads across our bones, joints and soft tissues. Sustained or repetitive end-range hip postures or movements will result in disproportionately high edge-loading (loading around the outer edge of the joint), and increased loads on the adjacent soft tissues. It’s simple physics really. Whether this disproportionate or excessive load ever results in tissue damage, pain or dysfunction is another matter. In the development of pathology, multiple factors are usually implicated, and different combinations of factors are at play for different individuals. There is also a well-accepted disconnect between pain and pathology.
And yet …
o Local tissue pathology and inflammation are associated with nociception
o Local tissue pathology and inflammation could be considered an important risk factor for the development of pain
Although pain and pathology are not well correlated, it does not follow that local pathology and nociception are irrelevant to the management of pain, particularly in the presence of irreversible pathology such as degenerative joint change. Providing targeted load management advice including postural and movement training, using appropriate dialogue does not need to induce hypervigilance but can instead for some individuals lead to rapid changes in pain, function, self-efficacy and quality of life.
As to the assertion that the body is robust and will simply adapt to overcome any loading scenario … there will always be a limit to what the body can adapt to and this limit will vary for each individual. It will depend on many other factors – genetics, morphology, general systemic health, musculoskeletal conditioning, prior injury etc. Commonly attached to the ‘body is robust’ argument is some example of a highly conditioned elite athlete with poor biomechanics. It does not translate that the deconditioned patient in front of us in the clinic, with genetic and morphological predisposition and a history of past injury, should be able to simply ‘adapt’ to adverse loading scenarios induced by their postural or movement strategies.
Load management is now a well-accepted strategy for management of musculoskeletal pain. If the issue is simply a training error – too much too soon – then of course, reducing training load and gradually building up again, allowing time for adaptation is an appropriate solution. However, if the relative overload is underpinned by habitual sustained or repetitive loads which have become part of natural postural and movement patterns or sporting technique, the problem is unlikely to be solved for the longer term by simply unloading and gradually reloading involved structures.
Case Scenario Application - Standing Posture and Hip Joint Loads
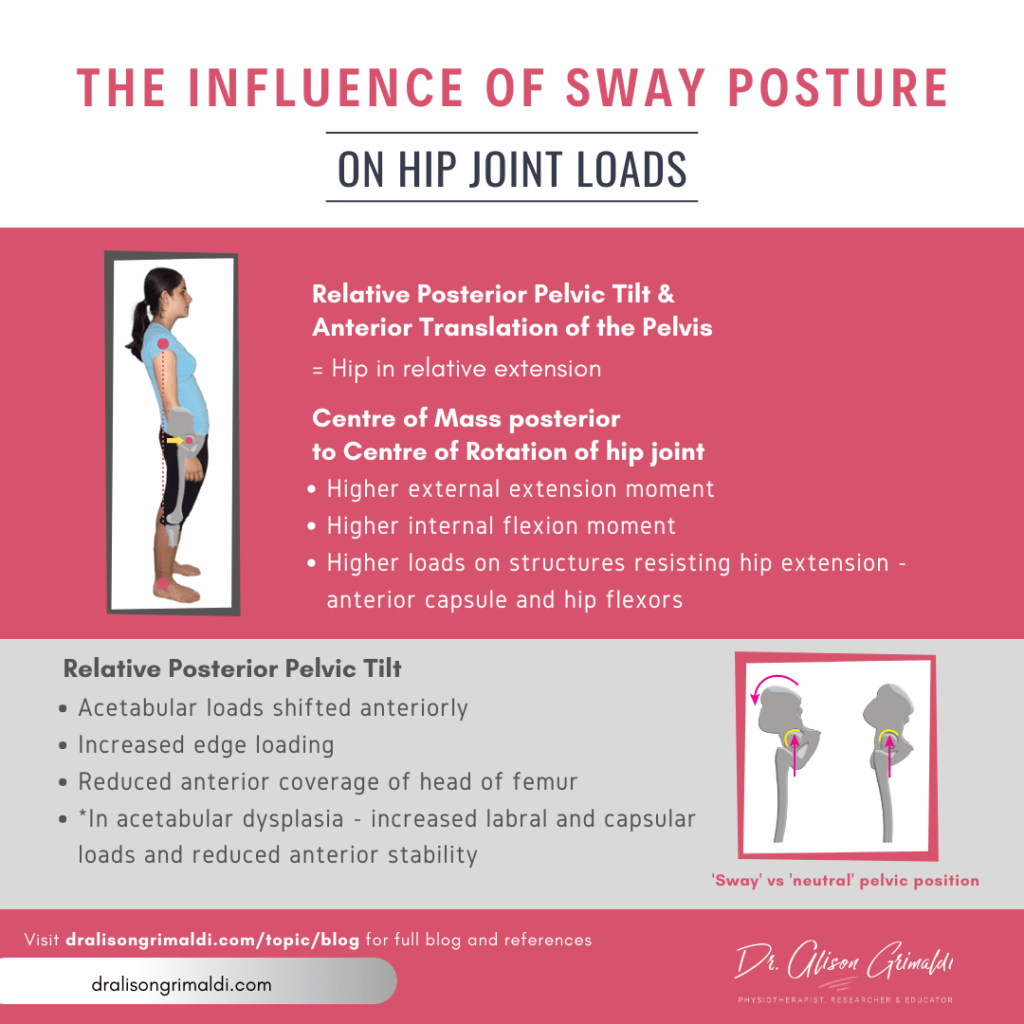
Let’s look at a specific example around the hip. Consider a young woman who presents with anterior hip pain in the context of mild acetabular dysplasia. Her pain is exacerbated by prolonged standing and walking, particularly walking at a fast pace or for more than 30 minutes. She aims to get her 10,000 steps per day, which usually includes a 30-45 minute walk but finds that if she’s been on her feet a lot during the day, her hip aches at night. On examination, you note she stands and walks in relative posterior pelvic tilt and anterior translation of the pelvis (often referred to as ‘sway’ type posture). She is positive on clinical tests for an intra-articular source of nociception.
What effect is this pelvic posture likely to have on our patient's anterior hip structures and hip joint loads?
While some say that standing posture has no relevance to dynamic function, pelvic posture in standing tends to strongly influence hip and pelvic mechanics in gait. I am yet to see someone in clinical practice who stands in a ‘sway’ (posteriorly pelvic tilted) posture and then suddenly flips into anterior pelvic tilt to walk.
How does walking in a sway posture influence kinematics and hip joint loads in gait?
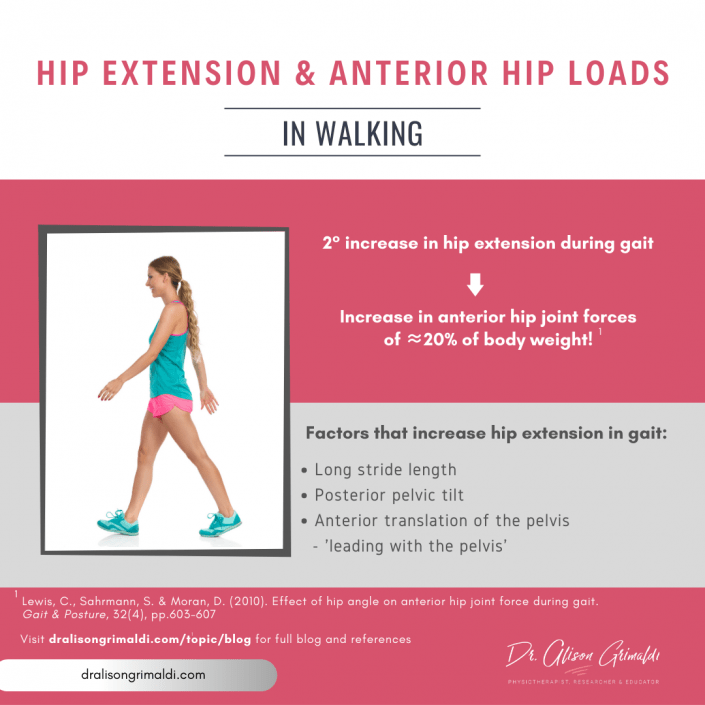
Lewis and Sahrmann1 provided insights here by collecting kinematic and force plate data during walking with different postures. Walking in the swayback posture resulted in a higher peak hip extension angle and a higher hip flexor moment (to resist the higher forces moving into hip extension) compared to natural posture. In previous research, these authors had already established that a 2° increase in hip extension angle resulted in a very meaningful increase in anterior hip joint forces of approximately 20% of body weight.2 Walking in a sway posture, in relative posterior pelvic tilt and anterior translation will therefore be key contributors to greater hip extension and higher anterior hip joint forces.
Another recent modelling study demonstrated that pelvic tilt significantly changes anterior acetabular loads. Shifting from 10° posterior pelvic tilt to 10° anterior pelvic tilt reduced anteriorly directed acetabular forces across the gait cycle by 29.3%.4 This change also altered hip muscle activity, reducing anterior hip muscle contributions and increasing posterior hip muscle contributions in walking. This has implications for both soft tissue and joint loading. The message here is not to think we need to ask people to suddenly change their pelvic position from dramatically, but to consider the impact that pelvic position may be having in an individual's pain presentation. For some, pelvic position may be irrelevant, but for others with extremes of pelvic position and a mechanical presentation, pelvic position may be critical.
The next steps are then around what to do about this - asking someone to just tilt their pelvis and hold in another position is unlikely to be successful and may cause different issues. Simple external cues can be used in movement training and exercise therapy can aim to work on mobility and relative 'balance' around the pelvis - relative flexibility and muscle strength-length.
Can modifying pelvic posture in gait alter hip pain & function?
For patients presenting with anterior hip pain who walk with a sway posture and/or excessive hip extension, reducing hip extension by altering pelvic posture and/or stride length through simple cues can have a marked and immediate effect on pain and function3. It will alsooften be appropriate to provide an exercise program to address muscle impairments and improve dynamic support of the anterior hip. However, if posture and gait patterns are not addressed, long term control of symptoms is less likely to be achieved with targeted exercise alone, particularly as most people will drop off with their exercise program once short-term pain relief is achieved. For appropriately selected individuals, using appropriately selected dialogue and cueing, postural and movement training can have marked and lasting positive effects.
Learn more about managing hip pain and the power of pelvic tilt within HIP ACADEMY.
References
1 Lewis, C. and Sahrmann, S. (2015). Effect of posture on hip angles and moments during gait. Manual Therapy, 20(1), pp.176-182.
2 Lewis, C., Sahrmann, S. & Moran, D. (2010). Effect of hip angle on anterior hip joint force during gait. Gait & Posture, 32(4), pp.603-607.
3 Lewis, C., Khuu, A. and Marinko, L. (2015). Postural correction reduces hip pain in adult with acetabular dysplasia: A case report. Manual Therapy, 20(3), pp.508-512.
Another great Anterior Hip Pain blog

Anterior Hip Pain: Causes & Contributing Factors
Adequate consideration of individual causes and contributing factors is important for best outcomes.