Adhesions after Hip Arthroscopy | Risk factors and diagnosis

In my last blog, we took a look at where adhesions after hip arthroscopy develop, what impact they may have, and the evidence around whether they are a problem or not. There are many reports that excessive post-operative adhesions are one of the most common reasons for failed hip arthroscopy and subsequent revision surgery.1,2,3,4,5 If you haven’t read the Part 1 of adhesions after hip arthroscopy, you might like to jump back there and have a scroll through the main points. In Part 2, we are moving on to discuss risk factors and diagnosis of adhesions after hip arthroscopy. Remember, next month we’ll jump into treatment and prevention of adhesions after hip arthroscopy in Part 3, so make sure you bookmark the page for the final instalment.
Discover our Anterior Hip & Groin Pain Course
If you enjoyed this blog, you might like to take the online course on Anterior Hip & Groin Pain - 5 hours of guided online video content. Better your skills and understanding of the anterior hip and groin and become equipped with the knowledge to administer clinical diagnostic tests and management strategies.
The topics we will be covering in Part 2:
What are the risk factors for developing post operative hip adhesions?
The risk of developing post-operative adhesions has been hypothesized to increase with more aggressive arthroscopic procedures, such as osteotomy (bone shaving) in those with FAIS, or in those who have undergone labral reconstruction.6 However, these factors have not been able to be clearly linked with risk of adhesions.3 It is evident that other factors, such as ‘who’ and what happens after surgery may be more impactful.3
Willimon and colleagues (2014) found that patients under 30 years of age were 5.9 times more likely, and patients who had Modified Harris Hip Scores below 50 were 2.4 times more likely to develop adhesions – identified at subsequent revision arthroscopy.3 The reasons are unknown, but it may have to do with the inflammatory status of the joint and/or aggressiveness or compliance with rehabilitation protocols - perhaps younger patients may push their rehab more aggressively and not allow as much time for recovery. In clinic, we find younger patients often tend to return to work more quickly.
Further evidence from this study supports a conclusion that post-operative factors may be more impactful than intra-operative factors, as those who did not perform hip circumduction exercises after surgery were 4.1 times more likely, and those who had microfracture as part of the hip arthroscopy procedure were 3.1 times less likely to develop adhesions.3

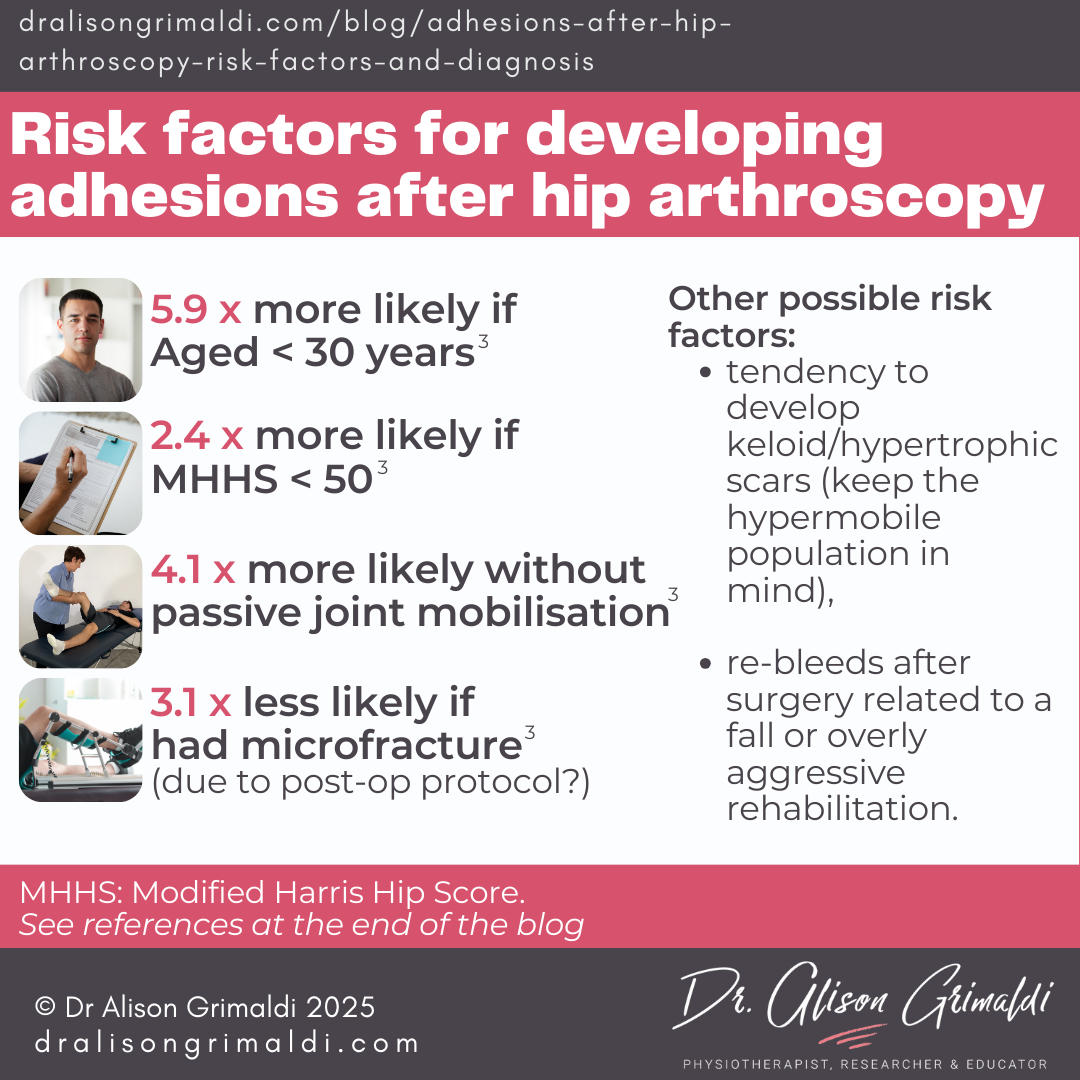
Microfracture involves using a small ‘pick’ to create bleeding of the subchondral bone, in areas of full-thickness cartilage loss. The aim here is to create fibrosis to fill the defect. Such a procedure would be expected to increase the risk of intra-articular adhesions; however, the opposite was true in this study. Why? The answer was suggested to be in the post-op care.
Patients who had microfracture used continuous passive motion (CPM) machines for 6 weeks post-operatively, instead of 2 weeks. In addition, microfracture patients had a longer period of protected weightbearing with crutches: 7–8 weeks (9.1 kg flat foot) compared to 3–4 weeks (9.1 kg flat foot) for those who did not have microfracture.3 Despite the aggressive intra-articular procedure, rates of problematic adhesions were lower due to the post-operative regime.
Other possible risk factors that have been suggested by experts in this area include a tendency to develop keloid/hypertrophic scars, re-bleeds after surgery related to a fall or overly aggressive rehabilitation.2

Want more? Gain access to all online hip courses, live and recorded masterclasses, Q & A sessions and Member Case sharing, and exclusive access to our entire how-to video library, ebook series and pdf resource library - diagnostic cheat sheets, condition info, management strategies & so much more.
Click here to find out how.
Diagnosis of post-operative hip adhesions
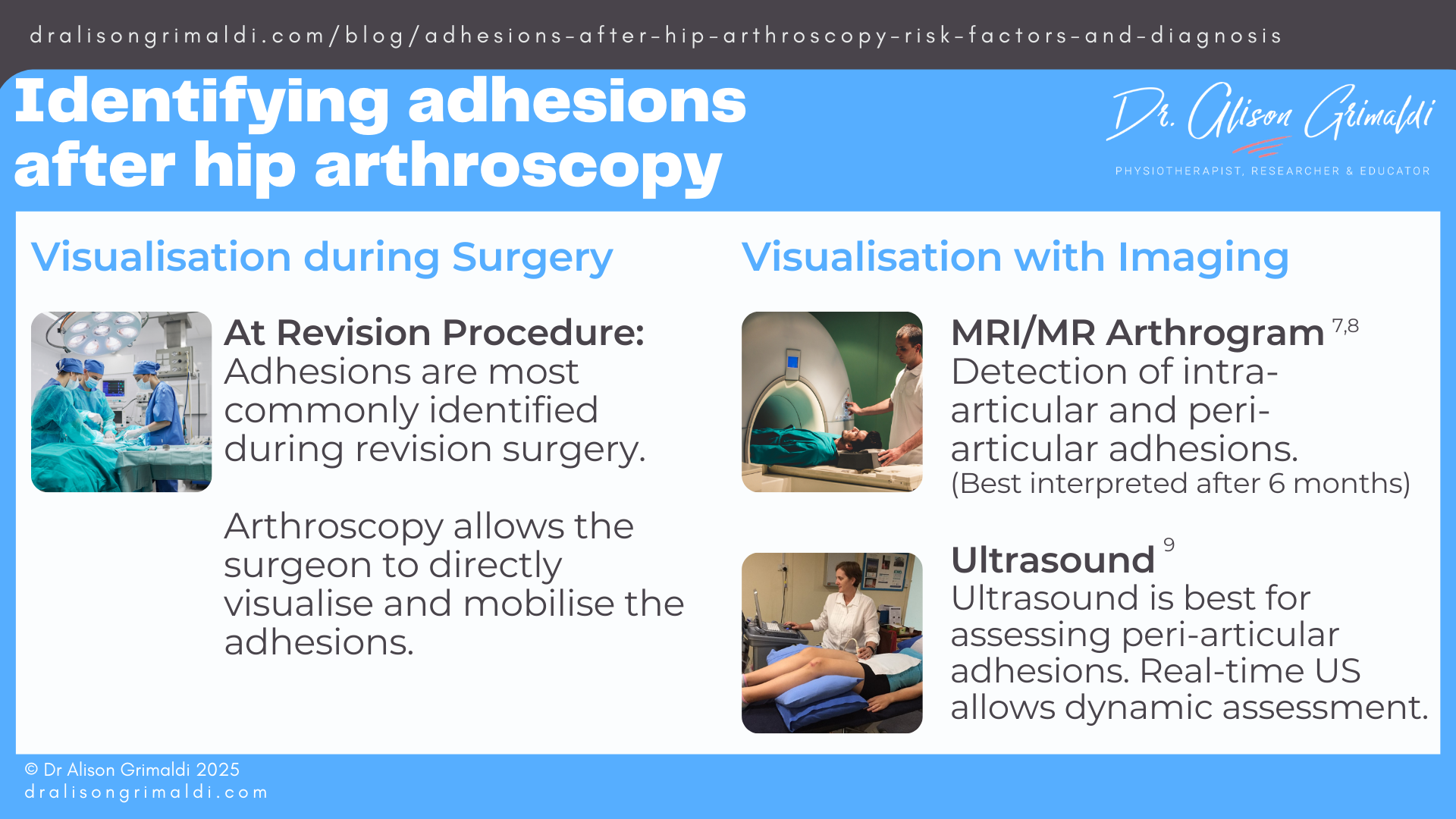
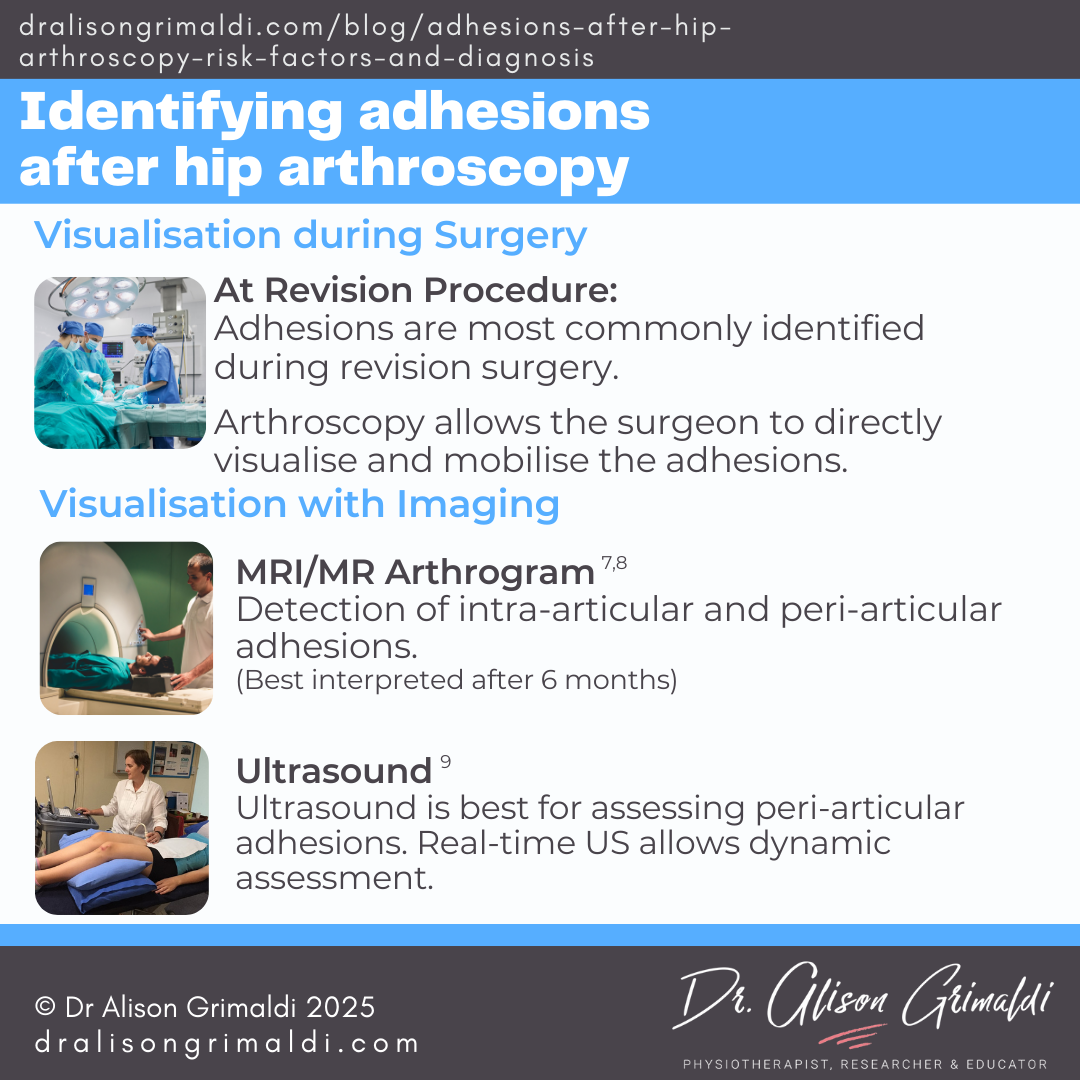
Visualisation at surgery or in imaging
In the available literature, post-operative adhesions have been most commonly identified at the time of revision surgery. Magnetic Resonance Imaging (MRI) can be useful,7 with obliteration of the paralabral sulcus and capsular adhesions to the femoral neck evident on MR arthrogram,8 although the extent of the adhesions or their impact may not be as readily appreciated as when directly visualised and manipulated in revision arthroscopy. Periarticular adhesions can also be identified on MRI or ultrasound.9 As adhesions are very common after arthroscopic surgery, the relevance must be considered on the basis of clinical presentation. Imaging may also be difficult to interpret in the first 3-6 months post-operatively.9
There are no clinical tests that allow us to determine the presence of adhesions with any degree of certainty, but certain symptoms and signs have been suggested to increase suspicion of a possible role of adhesions in the patient’s presentation.
Patient interview features of adhesions after hip arthroscopy
Features of a patient interview that are often linked with subsequent identification of adhesions during revision arthroscopy have been described by a couple of orthopaedic papers, with highly experienced senior authors.1,2
Common features within the patient interview include:
- persistent pain following surgery,
- feelings of “giving way” or catching,
- apprehension in attempting larger ranges of motion or particular actions,
- pinching/pain with flexion and/ or pulling with external rotation and extension
- usually a fairly positive early post-operative period, but discomfort with motion then increased, often around 10-16 weeks due to maturation of the scar tissue.2
It will also be important to understand physical loads applied to the hip in the early post-operative period. Was the hip exposed to very little early mobility? Did the patient delay rehab for a few weeks? Was the patient provided with early mobility work to complete? Was this completed regularly? Or is there any history of early post-operative trauma such as a slip or fall, or overly aggressive painful rehabilitation, often flaring pain for more than 24 hours?

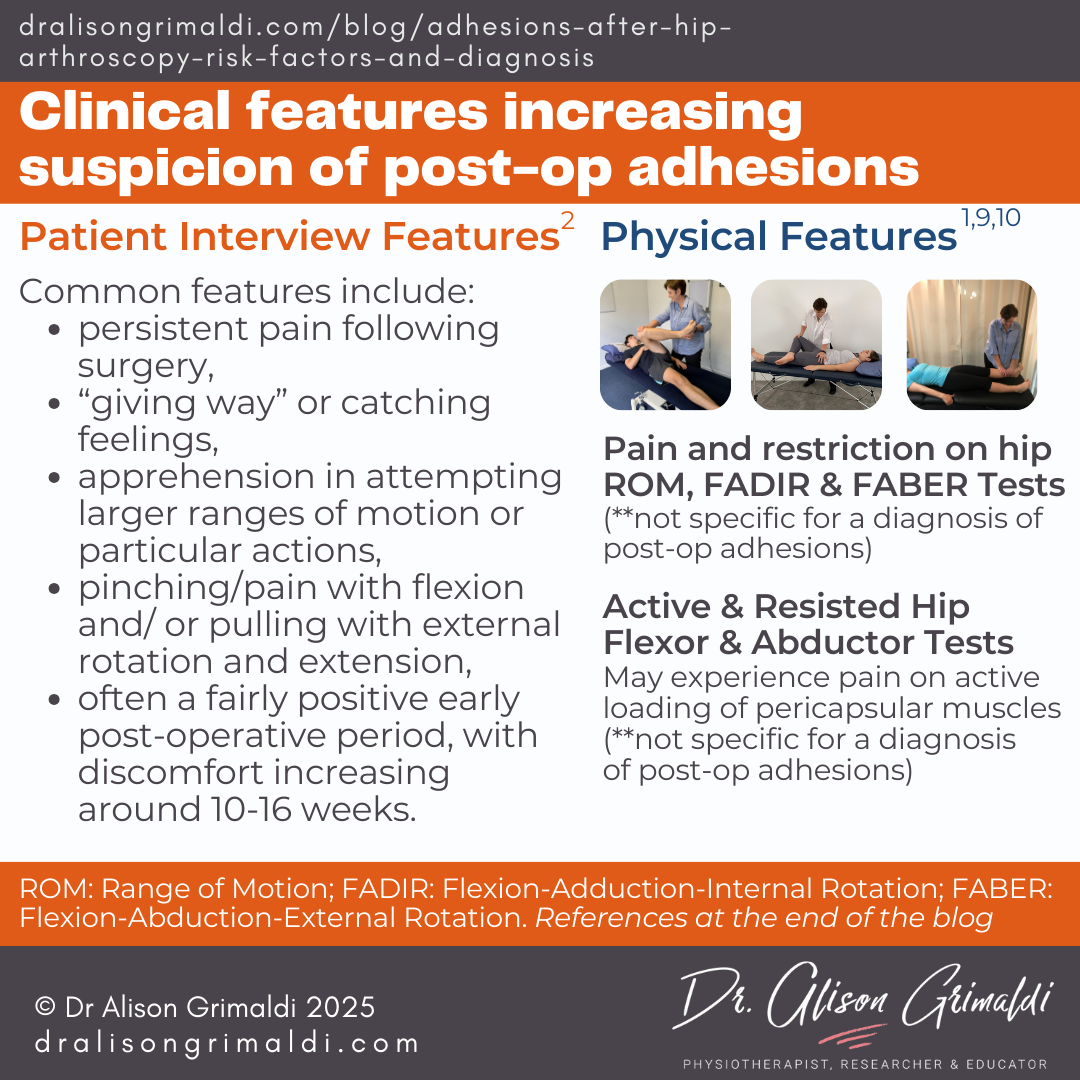
Physical features of adhesions after hip arthroscopy
The primary features of physical assessment reported in the literature relate to pain on loading and restricted range of motion.1,9 One study on periarticular adhesions after hip arthroscopy reported an indication for ultrasound guided treatments as: loss of range of motion in all planes more than 5° compared to the contralateral side, in addition to lack of any other clinically explainable cause of pain or limitation of hip movements.9
FADIR (hip impingement) and FABER (Patrick’s test) are usually included in the assessment.10 Pain and restricted motion on these tests may be related to many pathologies, which makes them most useful for helping rule out intra-articular pathologies, rather than indicating a particular source of pain. However, in a post operative patient, adhesions should be added to the possible differentials in those with pain and limitation on these tests.10
An extra flag that may increase suspicion of post-operative hip adhesions, is pain on mid-range active motion, that is not present during passive motion. Such a finding may be related to a source of pain in the musculotendinous tissues, however, pain on active loading may also indicate other sources of nociception that are loaded by active contraction of neighbouring muscles. The capsule and labrum may be loaded during active mid-range motion in those with micro-instability, but also in those with intra-articular or periarticular hip adhesions. If symptoms and other signs of microinstability are absent, adhesions may be more likely in the patient with a history of surgery or local trauma. The most likely active motions to be affected will be hip flexion and hip abduction.
If you’ve read Part 1 and now Part 2, you should now have a good understanding of the potential problems caused by adhesions after hip arthroscopy and now, risk factors and diagnosis of adhesions after hip arthroscopy. In this blog you can see that there are no specific tests that would accurately diagnose adhesions clinically, and even with visual assessment at the time of revision arthroscopy or on imaging, we can’t be sure that those adhesions are responsible for the pain and range limitations, or solely responsible for symptoms.
However, we have evidence that adhesions exist in people with persistent symptoms after hip arthroscopy, and it is certainly biologically plausible that such adhesions could contribute to post operative pain and restricted range. The impact of adhesions on joint protection mechanisms, as we discussed in Part 1, is also of concern regarding consequences for longer term joint health. So, it is reasonable to consider treatment and prevention strategies for adhesions after hip arthroscopy. Stay tuned for the next blog where we’ll be looking at these topics.

Have you heard about Hip Academy?
Transform the way you approach hip and buttock pain. Get the confidence to treat complex and challenging joint, tendon and nerve related pain.
With all Hip Courses included, enjoy all the extra inclusions, including; access to the entire eBook series, how-to video library, expanding PDF resource centre, live masterclasses, Q&A and Member Case Sharing sessions + a library of recordings!
Begin your Transformation!
Master Hip and Pelvic Conditions:
Gain expert knowledge and skills to assess and treat challenging hip and pelvic conditions with evidence-based methods.
Professional Growth:
Transform into a highly skilled hip specialist through structured learning and access to cutting-edge research and techniques.
Confidence in Practice:
Enhance your clinical confidence when dealing with complex hip issues, knowing you have the latest evidence and strategies at your fingertips.
Global Community Engagement:
Connect with a worldwide network of health professionals, exchanging ideas and learning from peers and experts in the field.
Continuous Learning:
Keep up with the latest advancements and research in hip physiotherapy, ensuring you stay at the forefront of your profession.

This blog was written by Dr Alison Grimaldi
Dr Alison Grimaldi is a physiotherapist, researcher and educator with over 30 years of clinical experience. She has completed a Bachelor of Physiotherapy, a Masters of Sports Physiotherapy and a PhD, with her doctorate topic in the hip region. Dr Grimaldi is Practice Principal of PhysioTec Physiotherapy in Brisbane and an Adjunct Senior Research Fellow at the University of Queensland. She runs a global Hip Academy and has presented over 100 workshops around the world.
Check Out Some More Relevant Blogs
References
- Ruzbarsky JJ, Soares RW, Comfort SM, Arner JW, Philippon MJ. Adhesions in the setting of hip arthroscopy. EFORT Open Rev. 2023 Nov 1;8(11):792-797.
- Philippon MJ, Ryan M, Martin MB, Huard J. Capsulolabral adhesions after hip arthroscopy for the treatment of Femoroacetabular Impingement: Strategies during rehabilitation and return to sport to reduce the risk of revision. Arthrosc Sports Med Rehabil. 2022 Jan 28;4(1):e255-e262. doi: 10.1016/j.asmr.2021.10.031. PMID: 35141559; PMCID: PMC8811550.
- Willimon SC, Briggs KK, Philippon MJ. Intra-articular adhesions following hip arthroscopy: a risk factor analysis. Knee Surg Sports Traumatol Arthrosc. 2014 Apr;22(4):822-5.
- Den Hartog TJ, Leary SM, Schaver AL, Parker EA, Westermann RW. The incidence and outcomes following treatment of capsulolabral adhesions in hip arthroscopy: A systematic review. Iowa Orthop J. 2023 Dec;43(2):146-155. PMID: 38213862; PMCID: PMC10777703.
- Keogh JAJ, Keng I, Ifabiyi M, Patel M, Duong A, Malviya A, Wuerz TH, Ayeni OR. Adhesions after hip arthroscopy are associated with revision but show poorly defined criteria for diagnosis and operative management: a systematic review. Arthroscopy. 2024 Apr 30:S0749-8063(24)00303-7. doi: 10.1016/j.arthro.2024.04.008. Epub ahead of print. PMID: 38697325.
- Locks R, Bolia IK, Utsunomiya H, Briggs KK, Philippon MJ. Revision hip arthroscopy after labral reconstruction using iliotibial band autograft: Surgical findings and comparison of outcomes with labral reconstructions not requiring revision. Arthroscopy. 2018 Apr;34(4):1244-1250. doi: 10.1016/j.arthro.2017.10.054. Epub 2018 Feb 15. PMID: 29456067.
- Woodward RM, Philippon MJ. Persistent or recurrent symptoms after arthroscopic surgery for Femoroacetabular Impingement: A review of imaging findings. J Med Imaging Radiat Oncol. 2019 Feb;63(1):15-24. doi: 10.1111/1754-9485.12822. Epub 2018 Oct 27. PMID: 30369089.
- Kim CO, Dietrich TJ, Zingg PO, Dora C, Pfirrmann CWA, Sutter R. Arthroscopic hip surgery: Frequency of postoperative MR arthrographic findings in asymptomatic and symptomatic patients. Radiology. 2017 Jun;283(3):779-788. doi: 10.1148/radiol.2016161078. Epub 2016 Dec 7. PMID: 27930091.
- M V Reddy S, Ayeni O, Vatturi SS, Yu H, Choudur HN. Ultrasound-guided release of post-arthroscopy extra-articular hip adhesions in femoroacetabular impingement: a novel technique. Skeletal Radiol. 2021 Dec;50(12):2541-2548. doi: 10.1007/s00256-021-03766-z. Epub 2021 Apr 12. PMID: 33844029; PMCID: PMC8038923.
- Gaio NM, Turner EHG, Spiker AM. Hip manipulation under anesthesia for post-hip arthroscopy pericapsular scarring: Indications and techniques. Arthrosc Tech. 2023 May 29;12(6):e983-e989. doi: 10.1016/j.eats.2023.02.036. PMID: 37424664; PMCID: PMC10323974.