Surgical and rehab predictors of failed hip arthroscopy
Can't make the workshop? Do the Online Course
Unfortunately, many people to continue to have pain and functional difficulty after hip arthroscopy. In my last blog we discussed patient predictors of failed hip arthroscopy - factors that are important to consider when deciding if a patient is likely to have a good outcome from arthroscopic surgery. So, the surgeon has selected the perfect patient for surgery, they should have an excellent outcome, right? Not necessarily. There are things that can happen, or things that don't happen, during or after the surgery that may also strongly influence outcomes. Surgical bone, labral and capsular management are important factors, and there is always a small risk of iatrogenic damage with any surgical procedure. Assuming the surgery goes well, this is just the first step in the recovery process, with rehabilitation usually spanning 3-6 months. There is much potential during this timeframe for patients and health professionals to alter the course of the recovery. In this blog, we'll cover surgical and rehab predictors of failed hip arthroscopy.
Surgical factors that predict failed hip arthroscopy
A number of studies have now identified surgical techniques or iatrogenic injury that may increase the risk of persistent pain following hip arthroscopy, in many cases linked to reduced joint stability.
Bone management factors that may increase risk of failed hip arthroscopy
Both under-resection and over-resection of bone have been cited as potential reasons for failed hip arthroscopy. One of the most common reasons cited for repeat arthroscopy is residual impingement, with surgeons seeking to address any residual cam or pincer impingement. However, over-resection of cam morphology has been reported to result in far more profound problems and a greater conversion rate to arthroplasty than under-resection.1 Acetabuloplasty, resection of the acetabulum rim, may also lead to poorer outcomes particularly in the context of acetabular dysplasia2 where decisions for resection may be made on a measurements taken in a single radiological plane. This is why it is so important for acetabular dysplasia to be considered a 3-dimensional deficiency. (Read more about the 3-D nature of dysplasia here.)
Post-operative acetabular deficiency may also occur in patients undergoing arthroscopy for Femoroacetabular Impingement Syndrome (FAIS). Acetabular rim resection is often performed for pincer impingement related to acetabular retroversion. Acetabular retroversion results in anterior over-coverage of the femoral head and concurrent under-coverage of the posterior femoral head. Resection of the anterior rim may leave that joint unstable with inadequate global coverage of the femoral head. The rationale for rim resection as a joint preservation procedure also remains questionable, with pincer morphology so far shown to be more protective than inducive of hip osteoarthritis.3
Labral management factors that may influence hip arthroscopy outcomes
Labral tear is the most common indication reported for revision hip arthroscopy4, while the management of labral pathology is one of the strongest surgical predictors of failed hip arthroscopy. Labral debridement, trimming off the labral tear, is still the most common method of surgical management of labral tears in clinical practice and yet is most likely to result in poor outcomes. One recent systematic review reported high rates of failure and re-operation for labral debridement (63.6% failure) and much lower rates of failure after labral repair or reconstruction (22.8% failure).2
While the labrum carries very little bodyweight in the non-dysplastic hip, it has an important role in joint protection and stability. The labrum seals the joint, creating a vacuum for stability and trapping fluid between the chondral surfaces to disperse impact load. A labral tear has been reported to result in a reduction of fluid pressurisation of 25%, whereas a partial resection reduces this by around 50%, Philippon suggesting that if the only option in an arthroscopy is labral debridement, leaving the tear alone might be a better option.5 A labral tear reduces the distraction force required to break the hip’s vacuum seal by around 25%.6 It also allows more play in femoral head movement, with increases in translation and rotation of the femoral head reported in the presence of labral tear. Debridement does not address this deficit. Research has demonstrated that surgical labral repair or reconstruction may provide substantial improvements in these parameters but the partial resection occurring during labral debridement is more likely to worsen these parameters.5,6
In those with acetabular dysplasia, the bony under-coverage is partially compensated by increased load transmission to the acetabular labrum. In response, the labrum may hypertrophy and is also at higher risk of pathology. Debridement of this hypertrophied labrum can be devastating for the dysplastic hip due to reductions in joint stability.7
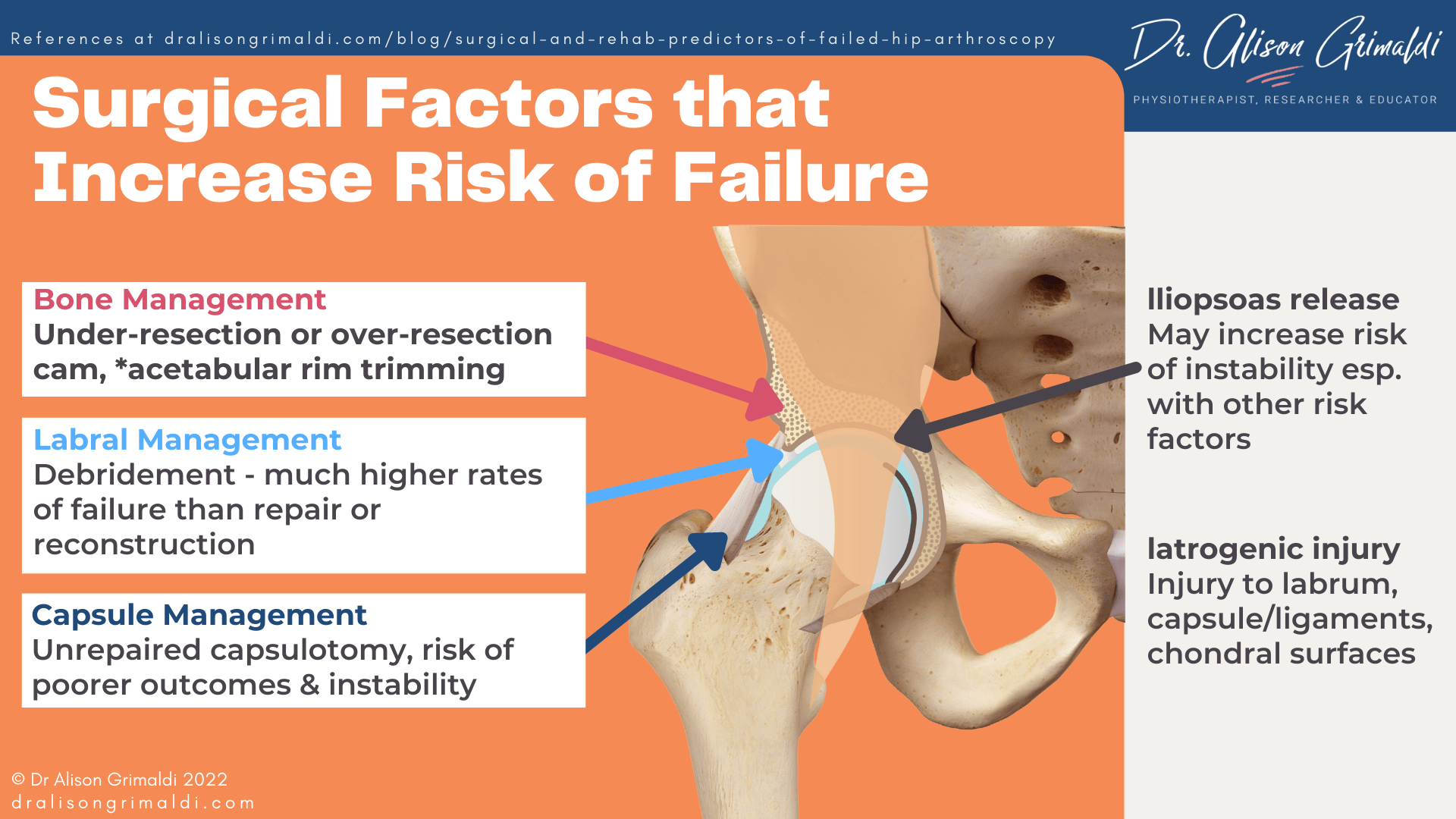
Capsular management factors that may contribute to persistent pain and instability following hip arthroscopy
The importance of capsular management has only been acknowledged more recently with building evidence to suggest that unrepaired capsulotomy is linked with poorer outcomes and instability with potential for anterior dislocation. In clinical practice a significant proportion of surgeons continue to leave the capsule open, and some even perform a partial capsulectomy – completely removing the anterolateral segment of the capsule for better exposure to the joint. There are case reports of instability following hip arthroscopy associated with capsular deficiency and sometimes sectioning and lack of repair of the iliofemoral ligament, critical to anterior hip stability. Although there is some mixed evidence, a recent systematic review investigated the effect of capsular closure on patient rated outcomes and demonstrated significantly higher mean postoperative scores and significantly superior improvement with repair.8
Capsular management remains the surgeon’s preference and it is unknown how many surgeons continue to leave the capsule unrepaired. For those health and exercise professionals providing post-operative rehabilitation following hip arthroscopy, it is important to access the operative notes or enquire of the surgeon if the capsule was repaired. This will better clarify risk of instability and potentially, impact on outcomes.
Those who have failed to recover after arthroscopy in association with iatrogenic capsular deficiency and instability usually present with persistent pain and mechanical symptoms such as clicking, locking and catching. Some will also report position-specific pain and a feeling that their hip will give way in weightbearing hip extension and external rotation.9 It is important for health professionals to have an awareness of these symptoms and the possibility of iatrogenic instability in those who fail or are slow to recover from arthroscopy.
Surgical capsular closure is likely to be particularly important for optimal outcomes for those with other factors predisposing to instability such as
- acetabular dysplasia,
- hypermobility spectrum disorders,
- concurrent surgical iliopsoas release,
- ligamentum teres rupture.
The impact of iliopsoas release on hip arthroscopy outcomes
The iliopsoas tendon and iliacus muscle belly are important anterior restraints for the hip joint. With the emergence of a theory of iliopsoas impingement causing labral tears just over a decade ago,10 we have seen a substantial increase in arthroscopic iliopsoas release – surgical sectioning of the iliopsoas tendon to varying degrees. It is often a procedure that is added during arthroscopy or offered after a failed arthroscopy, apparently more to cover all bases rather than as a specific treatment for a demonstrated impairment. Unfortunately removing the anterior support provided by the iliopsoas may increase the risk of instability post operatively,11 especially if combined with a lack of capsular closure and/or labral debridement and/or acetabular rim resection or dysplasia. As iliopsoas release also results in hip flexor weakness, it’s application particularly in younger patients or athletes should be carefully evaluated.12
Iatrogenic injury may contribute to poor outcomes after hip arthroscopy
Apart from the anticipated impact of procedures that are expected to occur or are planned within an arthroscopic procedure, there can be other unplanned iatrogenic injuries that occur during surgery. For example, placement of the portals is guided in most cases by fluoroscopy, but the actual advancement of the instruments occurs blind and is then checked after. During placement, the instruments may cause damage to previously pristine labrum or cartilage surfaces. Some surgeons have upskilled themselves to use real time ultrasound to place their instruments with full visualisation.13Damage to chondral surfaces and larger capsulotomies may also occur due to the tight space in which the arthroscopist has to work, particularly if the surgeon is learning or is a low-volume surgeon. Hip arthroscopy requires skill and experience to minimise risk of iatrogenic injury.
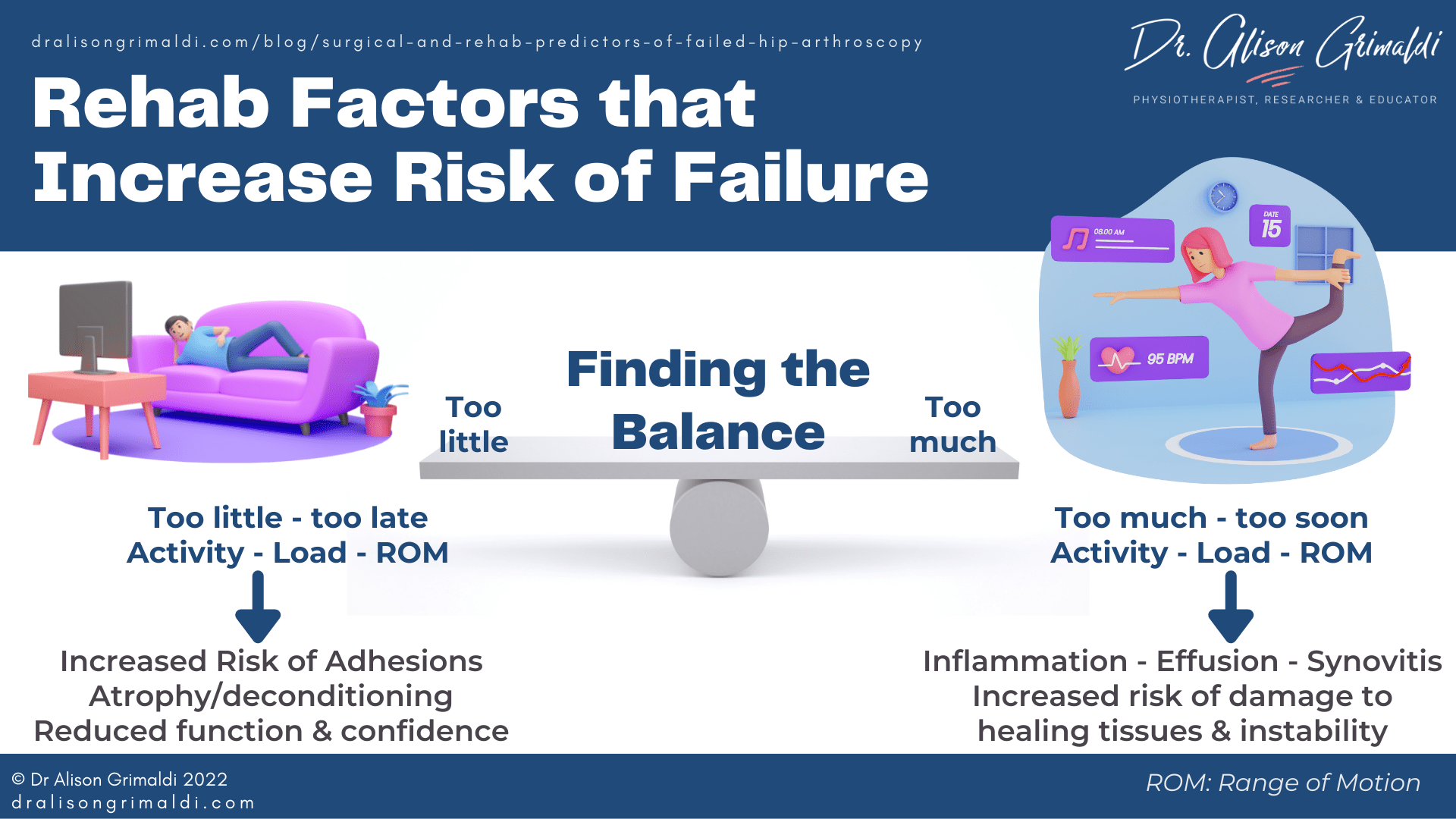
Rehabilitation factors that influence outcome of hip arthroscopy
Once the surgeon has completed the surgical intervention, the rehabilitation period begins. Things that happen or do not happen in this rehab period may alter the outcomes of surgery and contribute to failed arthroscopy. Unfortunately, while there are published rehabilitation protocols, there is a lack of evidence at this stage regarding best practice for post-operative care. The following information will therefore discuss some general considerations for how the post-operative period may impact on outcomes.
Trauma in the post operative period
There may be unanticipated events that occur in the post-operative period that impact on recovery. A slip, fall or other form of trauma within the first 10-16 weeks in which the capsule and any labral repairs are healing,14,15 may result in damage to the repaired tissues. This is one of the reasons that it is so important that patient safety on crutches is checked prior to discharge. Providing safety advice pre-operatively may also assist, by allowing the patient to ensure their home is as safe as possible for mobilising on crutches and then without aides in the first 10 - 16 weeks. For example, loose mats and rugs may need to be removed and a suction/non-slip mat may be useful in the shower.
Trauma to healing structures may also be caused inadvertently by overly aggressive passive mobilisation. It's important for clinicians to be aware of what was done in the procedure, abide by any restrictions provided by the surgeon and be mindful of ranges of motion that should be limited in the early post-operative period.
Lack of compliance with post-operative precautions
Unanticipated trauma to healing tissues may also occur within the healing period, due to failure of the patient to follow post-operative instructions. As the anterior capsule will be on stretch in hip extension and external rotation, forceful movements into end-range particularly when extension and external rotation are combined, may put the repaired tissue at risk. End-range flexion and flexion-internal rotation combinations will also place compressive and shear force across the anterior chondrolabral rim structures. Depending on the procedure, patients may be allowed to move through a painfree range or limited to 90degrees flexion for a period of time, usually the first 6 weeks or so of rehabilitation. Post-operative precautions will vary according to the procedure and surgeon.
Persistent synovitis may also contribute to ongoing pain following hip arthroscopy. Arthroscopy will induce an expected inflammatory response within the hip joint. This process will be most active in the first 6 weeks following surgery, which is why rehabilitation during this period usually focuses on gentle ranging (within appropriate range) and progressive but lower load exercises.16 Depending on the procedure and surgeon, there may be an initial period of non- or partial weighting and crutches are used for a variable period to allow protected weightbearing and function. Patients are also in this period usually instructed to avoiding vigorous weightbearing activity such as running, power-walking or jumping/landing tasks in the first 6 weeks or longer. Patients who do not follow the weightbearing and activity guidelines provided, may be more at risk of an exaggerated and/or extended inflammatory period. Increased inflammation is likely to contribute to pain and may also facilitate formation of excessive post-operative adhesions. Counselling our patients to avoid doing ‘too much-too soon’ may in the medium-long term ensure more rapid and optimal outcomes.
Lack of compliance with post-operative rehabilitation program
By the same token, it is not helpful for patients to be sitting around resting without attending to their rehabilitation program. Early and regular joint motion is extremely important for joint health and avoidance of post-operative adhesions and optimising return of range of motion. Active motion is also required to maintain and improve muscle function, dynamic joint support and functional capacity.
Post-operative rehabilitation and advice
The impact of the rehabilitation protocol is clearly not the sole responsibility of the patient. The health professional or rehabilitative team’s role is to ensure the patient is provided with clear instructions (and understands them) and a safe, evidence-informed, individualised program that aims to optimise post-operative outcomes.
Reducing Post Operative Adhesions
Rehabilitation aims to not only improve on pre-operative function, but to assist in minimising potential complications arising from the procedure. One of the most common complications leading to revision arthroscopy, is the formation of intra-articular and/or extra-articular adhesions.15 Adhesions form most commonly between the iliopsoas tendon and the capsule, and between the capsule and the labrum. Such adhesions are thought to contribute to persistent post-operative pain and limitations in range of motion. Severe adhesions of the capsule to the labrum may result in the tethered capsule lifting the labrum away from the femoral head during dynamic function, thereby releasing the hip fluid seal and reducing effectiveness of this natural joint protection/stability mechanism.15
Patients who have been identified to have severe capsulolabral adhesions during revision arthroscopy, had presented with persistent pain and common symptoms that include feelings of ‘giving way,’ catches of pain or pinching, pain with hip flexion and/or pulling with external rotation and extension movements.5 A lack of adequate early intervention to move the hip regularly in 3 dimensions, while avoiding overload of capsulolabral repair, may result in formation of adhesions.15,17 Some surgeons use continuous passive movement (CPM) machines routinely in their post operative protocols,15 but many prefer early active motion and mobility over hours of bed rest each day. CPM is not used routinely after hip arthroscopy in Australia. This means that the rehabilitation program needs to fulfil this goal of adhesion avoidance.
Passive mobilisation can be performed by the therapist and a partner at home. Passive circumduction is recommended by Dr Marc Philippon, 3 to 4 times per day, 30 repetitions clockwise and 30 repetitions counterclockwise for the first 10 weeks after surgery.15 It is a great option for a clinician to teach a partner some home circumduction. This can be a helpful adjunct. How much passive mobilisation is necessary and for how long is unclear. In situations where a clinician's face-to-face time with a patient may be limited by external factors, attention to the active exercise program, including self mobilisation will be a priority. The clinician should keep a close eye on range of motion to ensure range is not reducing from week to week and determine who requires more passive mobilisation.
Controlling oedema with compression shorts and passive soft tissue mobilisation may help to resolve swelling in the soft tissues. Patients can often perform gentle self-soft-tissue-mobilisation around the scar sites at home, to encourage movement of adjacent tissue layers. Early and regular active movement, at appropriate intensity, is likely to be most effective in preventing adhesions. Stationary cycling with no resistance and low speed usually starts within the first couple of days and active range of motion exercise should also be performed regularly from Day 1, with precautions in mind. Gentle active ranging (within limitations) in the pool, such as gentle cycling on a pool noodle can be useful and may be started as soon as 3-4 days post surgery. However, infection risk is a significant concern in the pool and if the effectiveness of a waterproof dressing is questionable, it may be better to delay until the wounds are closed at 10-14 days.
Restoring musculotendinous health and dynamic joint support
Persistent pain after hip arthroscopy may also be due to unresolved extra-articular sources of nociception and/or inadequate dynamic joint support from the surrounding muscles. Recent evidence has demonstrated that activation of deep hip musculature can reduce rim loading and change the direction of hip loading away from commonly damaged areas of acetabular cartilage.18 These muscles are often affected in those with joint related pain and may require targeted exercise, particularly in the early phases of rehabilitation.
A rehabilitation program needs to address any associated impairments in an appropriately progressed manner, adhering to precautions and monitoring exercise performance and symptom response. For return to higher level activity, patients will require a level of strength and kinematic control appropriate for the demand. A recent scoping review on exercise prescribed for FAIS reported that 48.6% of prescribed exercises were non weightbearing, 28.9% double leg, 22.5%, single leg and only 5% triplanar exercises.19 They concluded that such programs inadequately prepare the patient for functional demands, particularly in sport. There is inadequate evidence so far regarding superiority of any post-operative programs following hip arthroscopy, but the principles will be similar around the need for adequate progression of rehabilitative tasks for the patient’s needs. Performing higher level dynamic function with persistent impairments is likely to contribute to persistent symptoms following hip arthroscopy.
Other rehabilitation factors
There are other aspects of the rehabilitative process that are harder to separate and measure, such as the support and confidence provided by individualised contact with a therapist, and the beliefs of the patient around their condition and the importance of rehabilitation. A recent study exploring post-operative rehabilitation factors associated with outcomes and satisfaction reported that 1. frequency and length of individualised physiotherapy sessions, and 2. patient’s rating of the importance of home program/self-practice were significantly correlated with post operative HOS-ADL scores and level of satisfaction.20
With restrictions imposed by public health sectors and private insurers, funding for individualised care has been reducing over time, with many patients only receiving 5-6 sessions of post-operative treatment. Is this adequate? For some, maybe. For many others, maybe not, and this might be one important reason for the high rates of incomplete recovery that is reported in most studies. Future studies examining subgroups may in the future help identify those that need relatively more or less individualised support, for delivery of optimal and yet affordable outcomes within a stratified model of healthcare delivery. In the meantime, we need to measure and track impairments and outcomes and keep the lines of communication open with our patients, to deliver patient-centred care that aims to achieve best outcomes following hip arthroscopy.
If you are keen to hear more about rehabilitation considerations for hip arthroscopy, there is a wealth of information available within Hip Academy, including a recording of a recent member meeting - a 1 hour Hip Academy lecture and discussion on this topic.
Another great Anterior Hip Pain blog

Anterior Hip Pain: Causes & Contributing Factors
Adequate consideration of individual causes and contributing factors is important for best outcomes.
References
- Mansor Y, Perets I, Close MR, Mu BH, Domb BG. In search of the spherical femoroplasty: Cam overresection leads to inferior functional scores before and after revision hip arthroscopic surgery. Am J Sports Med. 2018 Jul;46(9):2061-2071.
- Shah A, Kay J, Memon M, Simunovic N, Uchida S, Bonin N, Ayeni OR. Clinical and radiographic predictors of failed hip arthroscopy in the management of dysplasia: a systematic review and proposal for classification. Knee Surg Sports Traumatol Arthrosc. 2020 Apr;28(4):1296-1310.
- van Klij P, Heerey J, Waarsing JH, Agricola R. The prevalence of cam and pincer morphology and its association with development of hip osteoarthritis. J Orthop Sports Phys Ther. 2018 Apr;48(4):230-238.
- Shapira J, Kyin C, Go C, Rosinsky PJ, Maldonado DR, Lall AC, Domb BG. Indications and Outcomes of Secondary Hip Procedures After Failed Hip Arthroscopy: A Systematic Review. Arthroscopy. 2020 Jul;36(7):1992-2007.
- Philippon MJ, Nepple JJ, Campbell KJ, Dornan GJ, Jansson KS, LaPrade RF, Wijdicks CA. The hip fluid seal--Part I: the effect of an acetabular labral tear, repair, resection, and reconstruction on hip fluid pressurization. Knee Surg Sports Traumatol Arthrosc. 2014 Apr;22(4):722-9.
- Nepple JJ, Philippon MJ, Campbell KJ, Dornan GJ, Jansson KS, LaPrade RF, Wijdicks CA. The hip fluid seal--Part II: The effect of an acetabular labral tear, repair, resection, and reconstruction on hip stability to distraction. Knee Surg Sports Traumatol Arthrosc. 2014 Apr;22(4):730-6.
- Makhni EC, Ramkumar PN, Cvetanovich G, Nho SJ. Approach to the patient with failed hip arthroscopy for labral tears and femoroacetabular impingement. J Am Acad Orthop Surg. 2020 Jul 1;28(13):538-545.
- Looney AM, McCann JA, Connolly PT, Comfort SM, Curley AJ, Postma WF. Routine capsular closure with hip arthroscopic surgery results in superior outcomes: a systematic review and meta-analysis. Am J Sports Med. 2021 Aug 17:3635465211023508. doi: 10.1177/03635465211023508. Epub ahead of print. PMID: 34403279.
- Shin JJ, de Sa DL, Burnham JM, Mauro CS. Refractory pain following hip arthroscopy: evaluation and management. J Hip Preserv Surg. 2018 Jan 18;5(1):3-14.
- Domb BG, Shindle MK, McArthur B, Voos JE, Magennis EM, Kelly BT. Iliopsoas impingement: a newly identified cause of labral pathology in the hip. HSS J. 2011 Jul;7(2):145-50.
- Sansone M, Ahldén M, Jónasson P, Swärd L, Eriksson T, Karlsson J. Total dislocation of the hip joint after arthroscopy and ileopsoas tenotomy. Knee Surg Sports Traumatol Arthrosc. 2013 Feb;21(2):420-3.
- Larson CM. Editorial Commentary: Psoas tenotomy in the setting of a borderline dysplastic hip risks iatrogenic instability: Be extremely cautious and particularly in athletes. Arthroscopy. 2021 Aug;37(8):2485-2487.
- Weinrauch P, Kermeci S. Ultrasound-assisted hip arthroscopy. Arthrosc Tech. 2014 Apr 3;3(2):e255-9.
- Philippon MJ, Arnoczky SP, Torrie A. Arthroscopic repair of the acetabular labrum: a histologic assessment of healing in an ovine model. Arthroscopy. 2007 Apr;23(4):376-80.
- Philippon MJ, Ryan M, Martin MB, Huard J. Capsulolabral adhesions after hip arthroscopy for the treatment of femoroacetabular impingement: strategies during rehabilitation and return to sport to reduce the risk of revision. Arthrosc Sports Med Rehabil. 2022 Jan 28;4(1):e255-e262.
- Naessig S, Kucharik M, Meek W, Eberlin C, Martin S. Prehabilitation and Rehabilitation Program for Patients Undergoing Arthroscopic Acetabular Labral Repair: A Comprehensive 5-Phase Patient-Guided Program. Orthop J Sports Med. 2022 Feb 8;10(2):23259671211071073.
- Philippon MJ, Ferro FP, Nepple JJ. Hip capsulolabral spacer placement for the treatment of severe capsulolabral adhesions after hip arthroscopy. Arthrosc Tech. 2014 Apr 21;3(2):e289-92.
- Meinders E, Pizzolato C, Gonçalves B, Lloyd DG, Saxby DJ, Diamond LE. Activation of the deep hip muscles can change the direction of loading at the hip. J Biomech. 2022 Mar 1;135:111019.
- Wright AA, Tarara DT, Gisselman AS, Dischiavi SL. Do currently prescribed exercises reflect contributing pathomechanics associated with femoroacetabular impingement syndrome? A scoping review. Phys Ther Sport. 2021 Jan;47:127-133.
- Amar E, Martin RL, Tudor A, Factor S, Atzmon R, Rath E. Midterm Outcomes and Satisfaction After Hip Arthroscopy Are Associated With Postoperative Rehabilitation Factors. Orthop J Sports Med. 2021 Jan 28;9(1):2325967120981888. doi: 10.1177/2325967120981888. PMID: 33614802; PMCID: PMC7869163.