1 of 12 Top Hip Papers of 2025 | Impact of FAIS Treatments on Hip Osteoarthritis Progression

Welcome to my 12 Top Hip Papers series of miniblogs for 2025, starting with this paper that explores how and if surgery or physio for Femoroacetabular Impingement Sydrome (FAIS) slows the progression towards hip osteoarthritis (OA).1 Hip arthroscopy is commonly offered as a 'hip preservation' procedure, but does hip arthroscopy for FAIS prevent OA - what does this new evidence tell us? - read on to find out.
Some of you might have joined me for my 12 Top Hip Papers of 2024 series last year - 12 papers from 2024 papers that contributed strongly to our understanding of hip conditions and/or the assessment or management of hip pain or injury. If you haven't already downloaded your free ebook of 12 top hip papers from 2024, you can do it by clicking HERE.
This year, I'll be focusing on helpful hip papers published in 2025. I am aiming to provide an overview of how the research has moved the hip space forward this year. I have prepared infographics and key learnings for each paper from 2025. Quick, but info-packed reads for this busy time of year.
SPECIAL Xmas Offer!
Read until the end to claim a very special Christmas offer I have prepared just for you!
LIMITED TIME ONLY! ENDS MIDNIGHT 24th DECEMBER
1 of 12 Top Hip Papers of 2025: Does surgery or physio for FAIS slow the progression towards hip osteoarthritis?
Background:
- A randomised clinical trial (RCT) comparing outcomes of surgery and physiotherapy for Femoroacetabular Impingement Syndrome.
- The primary end-point for patient rated outcomes (HOS-ADL) was set for 8 months and has been reported previously.
Study Aim:
The aim of this project was:
- to report the primary end-point of radiographic OA progression, and
- to report HOS ADL scores at 38 months post-randomisation.
What was done:
Method:
- Participants were randomised into 2 treatment groups:
In this RCT for FAIS, 222 participants (mean age 36.2 (18-60) years; 66% female) were randomised to have either hip arthroscopy with 4 post-operative physiotherapy sessions, or physiotherapy alone (maximum 8 sessions allowed but on average participants completed only 6 sessions).
Hip arthroscopy:
- Labral/chondral surgery and bony reshaping (osteoplasty)
- + Post Op Rehabilitation: 4 sessions
- Focused on optimising ROM and graded return to activity
- Active ROM, isometric exercise, stretching, exercise bike
- Progress to strengthening and low impact exercise
- Impact tasks introduced at 6 weeks
- Sports-specific rehabilitation as appropriate
Physiotherapist Led Rehabilitation:
- Average of 6 sessions (max 8)
- Included advice to avoid extremes of Flexion, Abduction, and Internal Rotation
- Focused on muscle strengthening to improve core stability and movement control (no other specifics)
- Encouraged a home exercise program (adherence unknown)
Key Findings:
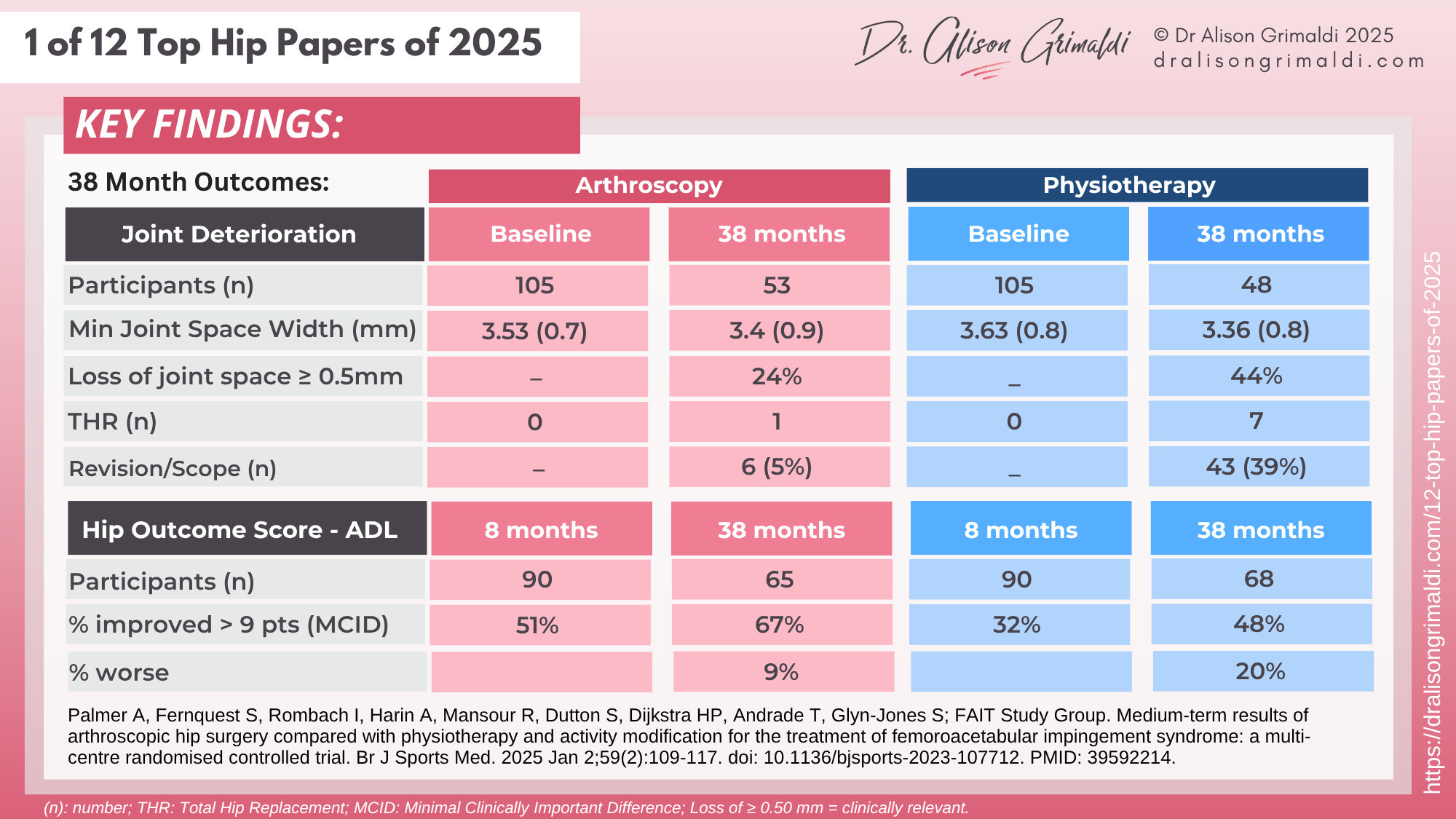
The primary 38-month outcome of this RCT assessed change in minimum joint space width between groups, aiming to test if hip arthroscopy (with post-op rehab) slows the progression of hip osteoarthritis more than physiotherapy alone. The primary outcome measure to assess change in symptoms was the Hip Outcome Score (ADL subscore) - the HOS-ADL.
Summary:
- Does hip arthroscopy for FAIS prevent OA? No significant difference in minimum Joint Space Width was seen between groups 38 months post hip arthroscopy or physio.
- A Magnetic Resonance Imaging (MRI) scoring system (SHOMRI) showed there was more progressive joint degeneration in the physiotherapy group than in the arthroscopy group, although the clinical significance is unclear.
- Surgery remained statistically superior to physio in reducing symptoms (HOS-ADL) at 3 years post-randomisation. However, the difference did not reach a threshold for clinical importance.
Limitations:
- There was a high loss to follow up which introduces significant bias. There was no data available for around half of the participants for xray assessment and almost 30% did not have HOS-ADL score at 38months.
- There were high cross-over rates, with 39% of the physio group crossing over to have surgery.
- As noted by the authors, the physio intervention ‘does not necessarily reflect best practice, which may have influenced patient outcomes’. Only 6 treatments were received on average, with unknown compliance, no follow up and poor detail around the intervention provided.
Clinical Implications:
- It is still uncertain if differences in joint health and patient rated outcomes between the groups equates to a meaningful therapeutic benefit for arthroscopy over physiotherapy in the longer term.
- A trial of high-quality physiotherapy for FAIS is warranted.
- The decision to operate for FAIS should be made around symptom improvement rather than prevention or delay of hip OA.
This RCT has been one of the best attempts so far to address the question of whether osteoplasties of the femoral neck or acetabulum are truly 'joint preservation' procedures. The outcomes are certainly not convincing here, with the authors concluding that at this point, the decision to operate for FAIS should be made around symptom improvement, rather than offered as a mechanism to prevent or slow the progression of hip osteoarthritis.
The large loss to follow up for the 38 month follow up highlights the difficulties of longer term studies, with 30-50% of participants unavailable for reassessment. This introduces substantial bias and makes it difficult to draw conclusions, because we don't know if a large proportion of those participants that did not return had a poor result, or alternately an excellent outcome.
The other major issue with surgery versus physio comparisons, is that 6 sessions of physio with no treatment details or compliance data, does not reflect 'best non-surgical practice.' In addition, the operative group received almost as many physio sessions, which does make comparisons unclear. This is a challenge for these types of studies, because post-operative rehabilitation is of course necessary and I would certainly recommend more than 4 sessions in a post surgical group, so neither of these scenarios may represent optimal care.
Overall, this study tells us that there is still insufficient evidence to recommend surgery to prevent or slow hip OA for FAIS. Between-group symptom differences were not clinically important. High quality hip rehabilitation should be trialled prior to surgery, but hip surgery is an option if symptom control is insufficient.

SPECIAL HOLIDAY OFFER!
$100 OFF
your Hip Academy joining fee
Offer Only Available During the 12 Hip Days of Christmas (13th-24th December). Do not miss this exclusive offer!
Now only AUD $345 (usually $445) to join to receive immediate access to over $4,800 worth of content!!
(AUD$345 equates to approximately 181 GBP and 230 USD)
USE COUPON CODE: xmas25hip
Like to learn more about managing labral tears and Femoroacetabular Impingement Syndrome?
In this course, you can find detailed information on pathoaetiology, assessment and management of hip joint related pain (including labral tears and FAIS), and many other conditions. To learn more, take the online course, or join me in an online or face-to-face workshop.
This online course is included in Hip Academy and Hip Academy members receive discounts for online workshops.
I hope you enjoyed the infographic and key learnings from Day 1 of my 12 Top Hip Papers of 2025. There are 11 more papers in this series, so keep an eye out for day 2 below, to see what other top papers and infographics I have prepared for you!