Acetabular Dysplasia: Development and Prevention

In the last couple of blogs, I’ve been examining what we know about important bony risk factors for hip pain and pathology – cam morphology and femoral malversion. Now we turn out attention to one other major morphological challenge for hip joint health, acetabular dysplasia. While hip dysplasia in adults has received far less attention than cam morphology and femoroacetabular impingement over the last decade or so, its impact can be devastating and far reaching. And, of all these morphologies, it may be the ‘easiest’ to prevent as we have much more awareness of when and how it develops and what we can do about it. Join me as I walk you through what we know about development of acetabular dysplasia, it’s impact and prevention strategies.
These are the topics we’ll be covering in this blog:
The impact of acetabular dysplasia
Natural development and change in acetabular shape through growth
Discover our Anterior Hip & Groin Pain Course
If you enjoyed this blog, you might like to take the online course on Anterior Hip & Groin Pain - 5 hours of guided online video content. Better your skills and understanding of the anterior hip and groin and become equipped with the knowledge to administer clinical diagnostic tests and management strategies.
Defining acetabular dysplasia
Dysplasia simply refers to abnormal growth. Hip dysplasia may be used to encompass abnormal growth of the acetabulum or proximal femur, so we’ll mainly be using the term acetabular dysplasia, referring to development of the acetabular socket.
Often acetabular dysplasia is defined in 2-dimensional terms, using only traditional indices such as the centre-edge angle, which measures the degree of acetabular coverage of the femoral head in a single plane – most commonly coronal or sagittal planes. However, the acetabulum is of course a 3-dimensional structure, and 2-D measures may miss or underestimate structural deficiency and potential impact of an individual’s morphology.1
There is a plethora of different ways to measure acetabular shape or gauge stability, in addition to the centre-edge angle. These include Roof Angle, Acetabular Index, Sharp’s Angle, Femoral head Extrusion Index, Anterior Wall Index, Posterior Wall Index, the Femoro-Epiphyseal Acetabular Roof Index (FEAR), and a new measure, the Gothic Arch Angle.

Want to get better at assessing hip xrays, including assessment of acetabular shape?
Join Hip Academy and you will have immediate access to:
- A 6-page A4 PDF resource to download and use as a cheat-sheet when you are next looking at a patient’s images
- The recording of an exclusive 45-minute lecture & discussion on Deciphering Hip XRays, presented to the Hip Academy community.
- The Hip Academy Video Library of techniques, that includes 7 x 1-2 minute videos walking you through exactly how to complete key Xray measures within an image viewing system (PACS). Watch and copy the steps while assessing your patient’s images.
All these measures can become a little overwhelming for many clinicians, so for this blog, let’s take the approach suggested by Wilkin and colleagues (2017) in their proposal of a contemporary model for defining acetabular dysplasia and structural instability.
They denoted 3 classifications – Anterior, Posterior and Lateral or Global Instability.1 These categories are used to define structural deficiency of the acetabulum, together with signs and symptoms of instability. I have written more detail about this system in a previous blog that you can find here.
Thinking of acetabular dysplasia in these categories can help with directing clinical assessment and particularly management – those with focal anterior acetabular deficiency will need a different approach to a patient with focal posterior or global deficiency of the acetabulum.
Typical or normal acetabular shape
The typical human acetabulum is a bony cup that sits in the lateral pelvis that houses the femoral head and forms the hip joint. The radius of curvature of this cup is usually similar to that of the femoral head, to provide a snug fit for stability. The acetabulum usually covers around 75% of the femoral head.2
The opening of the cup typically faces downward and anterolaterally. If you imagine an upside-down cup with the opening facing the floor, the typical cup is then angled up laterally 33-38° (Sharp or Sharp’s Angle)3 and anteriorly around 15-20° from the coronal plane (acetabular anteversion).2
Normal acetabular anteversion means that the femoral head is relatively less covered anteriorly than posteriorly, which is why we have a lot more range of motion in hip flexion than hip extension. While anterior wall coverage of the femoral head is typically around 19%, posterior wall coverage is around 43%,4,5 with the posterior wall of the acetabulum crossing around the centre of rotation of the femoral head.
The lateral centre edge angle (see figure below) is commonly used as a measure of lateral or global coverage of the femoral head. The typical hip has a lateral centre angle of 25-40°.
Acetabular Dysplasia - Anterior Deficiency
Those with focal anterior acetabular wall deficiency have a normal lateral centre edge angle, but anterior wall coverage of less than 15% of the femoral head. Focal anterior wall deficiency occurs most commonly when the acetabulum is excessively anteverted – facing more forward than typical.
Excessive acetabular anteversion results in anterior undercoverage and posterior overcoverage. The posterior wall may then cover more than 50% of the femoral head, crossing laterally to centre of the femoral head.
Those with excessive acetabular anteversion and focal anterior wall deficiency are at higher risk of anterior hip instability and posterior impingement.
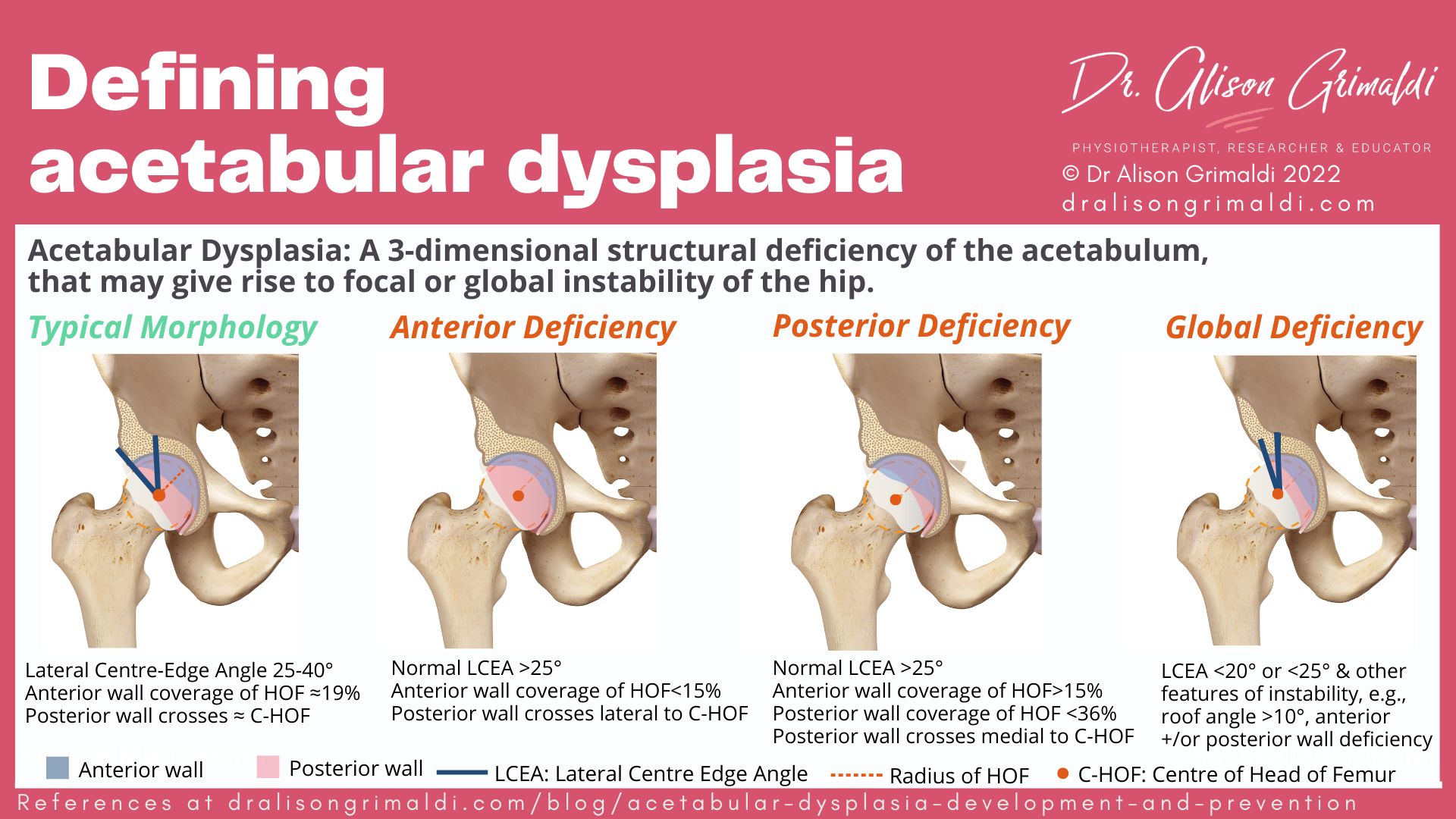
Acetabular Dysplasia - Posterior Deficiency
Those with focal posterior acetabular wall deficiency have a normal lateral centre edge angle, but posterior wall coverage of less than 36% of the femoral head. Focal posterior wall deficiency occurs most commonly when the acetabulum is retroverted – facing less forward than typical.
Acetabular retroversion results in posterior undercoverage and anterior overcoverage. The posterior wall may then usually cross medially to centre of the femoral head. This is referred to as the Posterior Wall Sign, indicative of reduced posterior coverage of the femoral head.
Those with acetabular retroversion are at higher risk of anterior femoroacetabular impingement (Pincer FAI) and posterior overload or instability.
Acetabular Dysplasia - Global Deficiency
Those with global acetabular deficiency have a lateral centre edge angle of <20° or <25° with other features of instability,1including anterior and/or posterior wall deficiency. Those with global deficiency are most likely to experience symptoms of hip instability.
The impact of acetabular dysplasia
Acetabular dysplasia and hip osteoarthritis
Acetabular dysplasia is one of the leading causes of hip osteoarthritis (OA), present in 20-40% of patients with hip OA.6 Reduced weightbearing surface and/or orientation of the acetabulum results in increased shear forces and edge loading (loading around the edge/rim of the joint).
Increased edge loading has been demonstrated to be significantly higher in those with acetabular dysplasia than in those with typical morphology:
- in the antero-superior acetabulum during gait,7 and
- in the posterior acetabulum rim during a deep squat.8
This edge loading will be influenced by an individual’s specific bony deficiency, as well as movement and muscle factors.7
Increased edge loading increases load on the acetabular labrum. Henak and colleagues (2011) demonstrated that the acetabular labrum needs to support 4-11% of the total load transferred across the joint in those with acetabular dysplasia, compared with only 1-2% in those without dysplasia.9
While the labrum usually adapts and hypertrophies, eventually the loads may surpass the physiological tolerance of the labrum and rim cartilage. Radiographic signs of osteoarthritis develop in 25-50% of those with dysplasia by the age of 50.6
Early development of symptoms may be related to a combination of factors – severity of bony deficits, functional demands, and movement and muscle impairments.
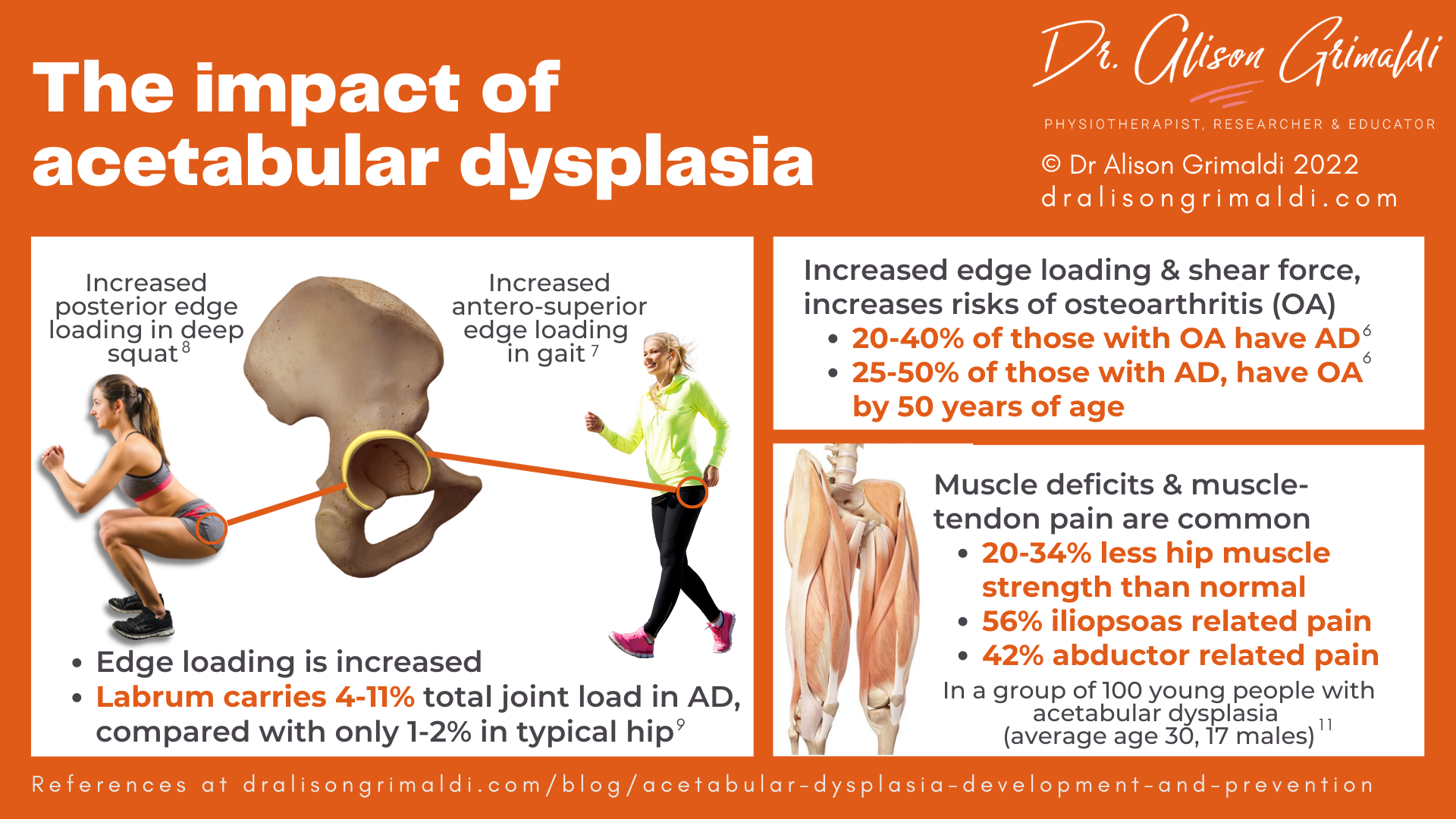
Acetabular dysplasia and muscle impairments
Those with acetabular dysplasia have been shown to have muscle impairments, with strength deficits of 20-34% in the hip musculature reported in patients prior to periacetabular osteotomy.10 Muscle-tendon related pain was also present in around half of this cohort of 100 patients with dysplasia (average age 30, 17 males). There was a high prevalence of muscle-tendon-related pain in the iliopsoas and the hip abductors, which impacted on strength and self-reported hip disability.11
Acetabular dysplasia is a 3-dimensional structural deficiency of the acetabulum, that may give rise to focal or global instability of the hip.
Natural development and change in acetabular shape through growth
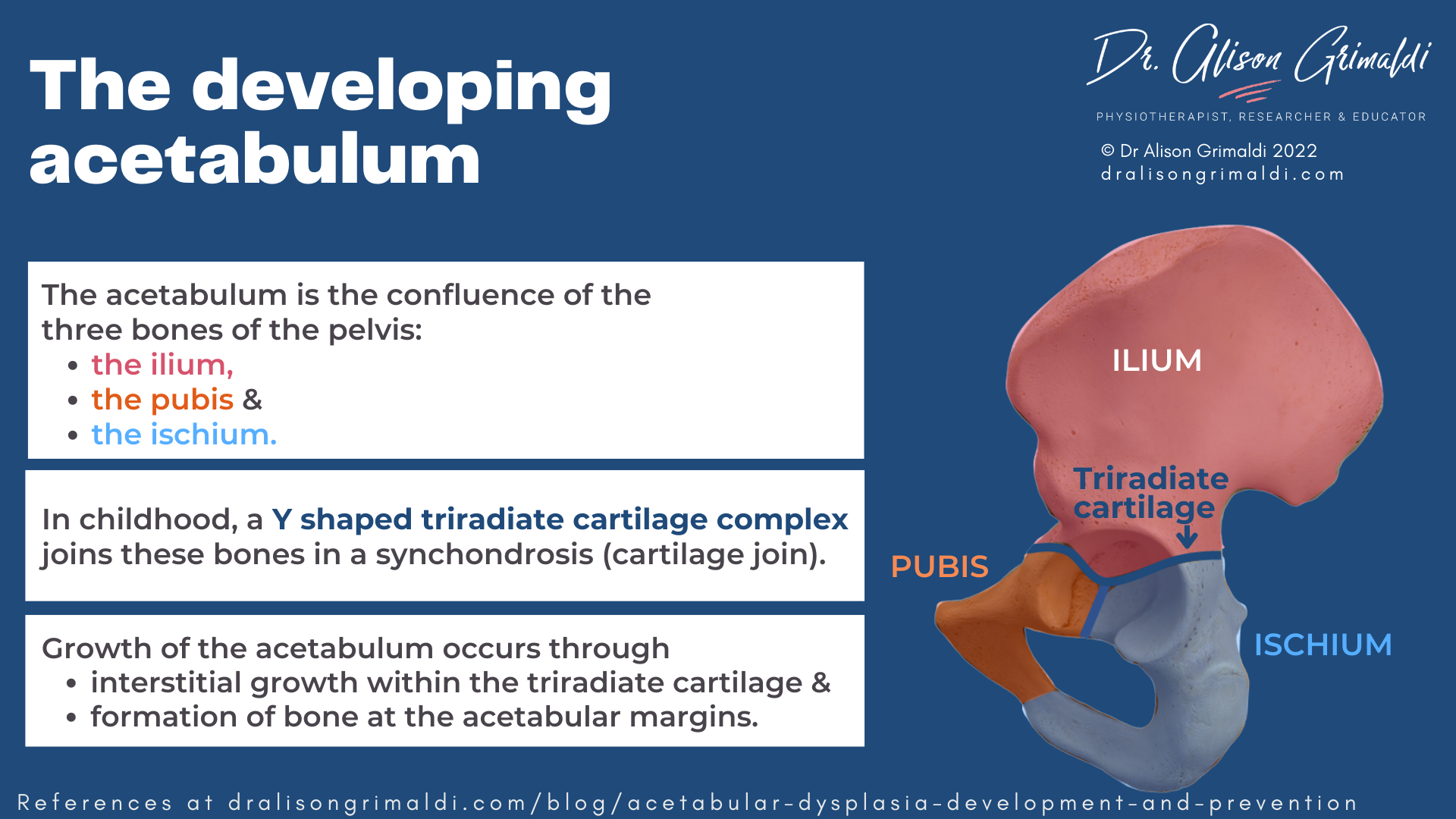
The acetabulum is formed by the joining of the 3 pelvic bones – the ilium, ischium and pubis. At birth, this confluence is not bony but cartilaginous. The Y shaped triradiate cartilage complex joins these bones in a synchondosis (bones joined by cartilage).
The iliac ossification centre forms superior acetabular bone, the pubic ossification centre (os acetabuli) forms the anterior wall of the acetabulum, and the ischial growth centre forms the posterior wall.12 Growth of the acetabulum occurs through interstitial growth within the triradiate cartilage and formation of bone at the acetabular margins.13
The triradiate cartilage ossifies in adolescence, with the posterior wall of the acetabulum ossifying more slowly, just before closure of the triradiate cartilage.14 Females reach bony maturation earlier, with ossification occurring around age 13. Closure of the triradiate cartilage in males doesn’t occur until a couple of years later, most ossifying around 15 years of age or a little later, with all growth completed by 18 years.13
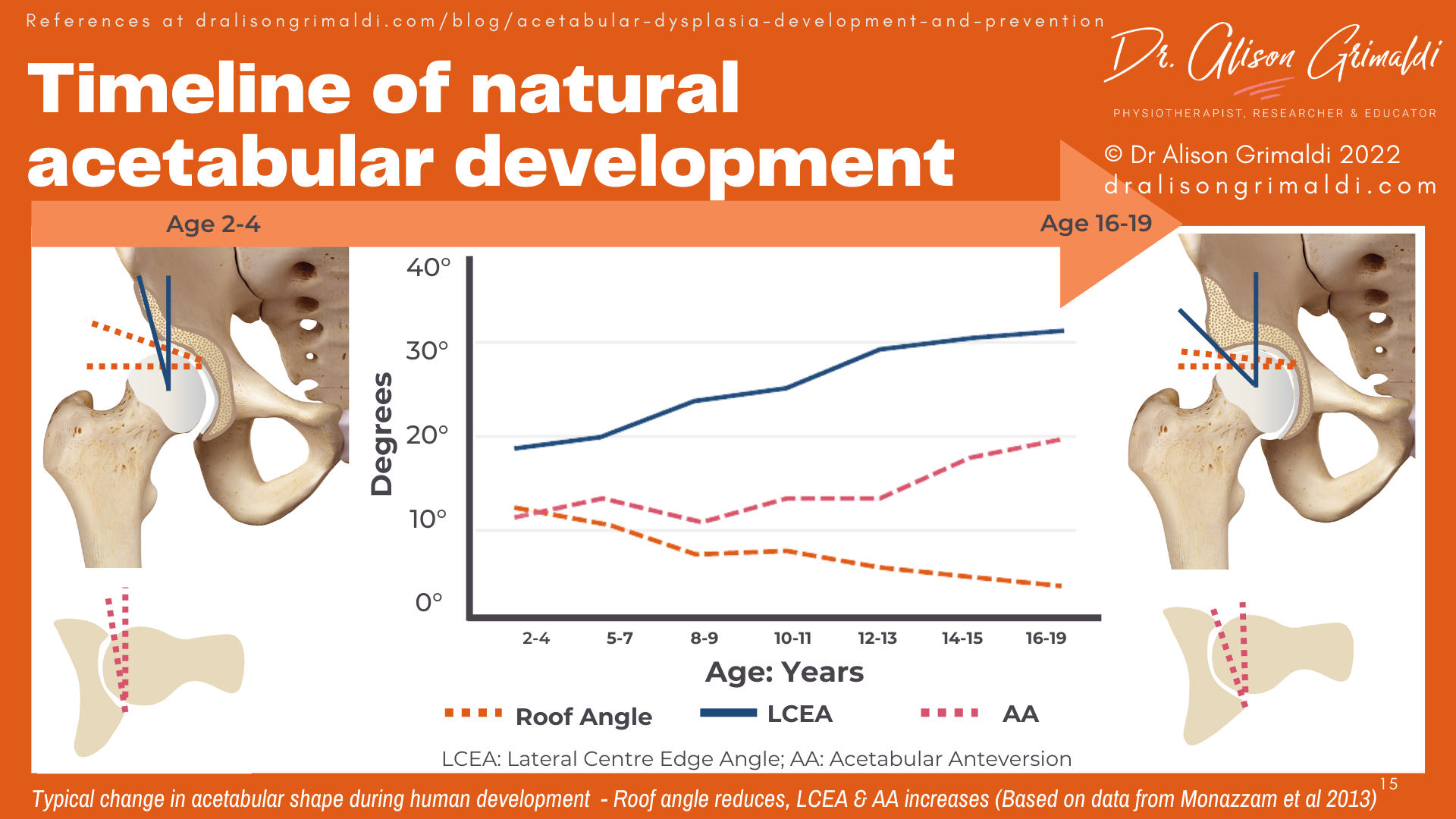
With growth of the acetabulum during childhood, the shape and orientation of the bony hip socket change. Monazzam and colleagues (2013) provided imaging evidence of differing acetabular indices across childhood and adolescence, from age 2 to 19 years.15
As you can see in the infographic below, roof angle reduces and lateral centre edge angle (lateral coverage of the femoral head) increases during growth, thereby increasing joint stability.
Acetabular version also changes, with the acetabulum only angled forward 11.5° in early childhood but reaching 20.1° in Monazzam et al’s cohort by adulthood (measured at the centre of the femoral head).15 There is a fairly rapid change increase in version just prior to the ossification of the triradiate cartilage in adolescence. Because the posterior wall continues to grow a little more after the anterior wall has ossified, the acetabulum will end up relatively facing further forward – check the infographic below to visualise this change.
Causes of acetabular dysplasia
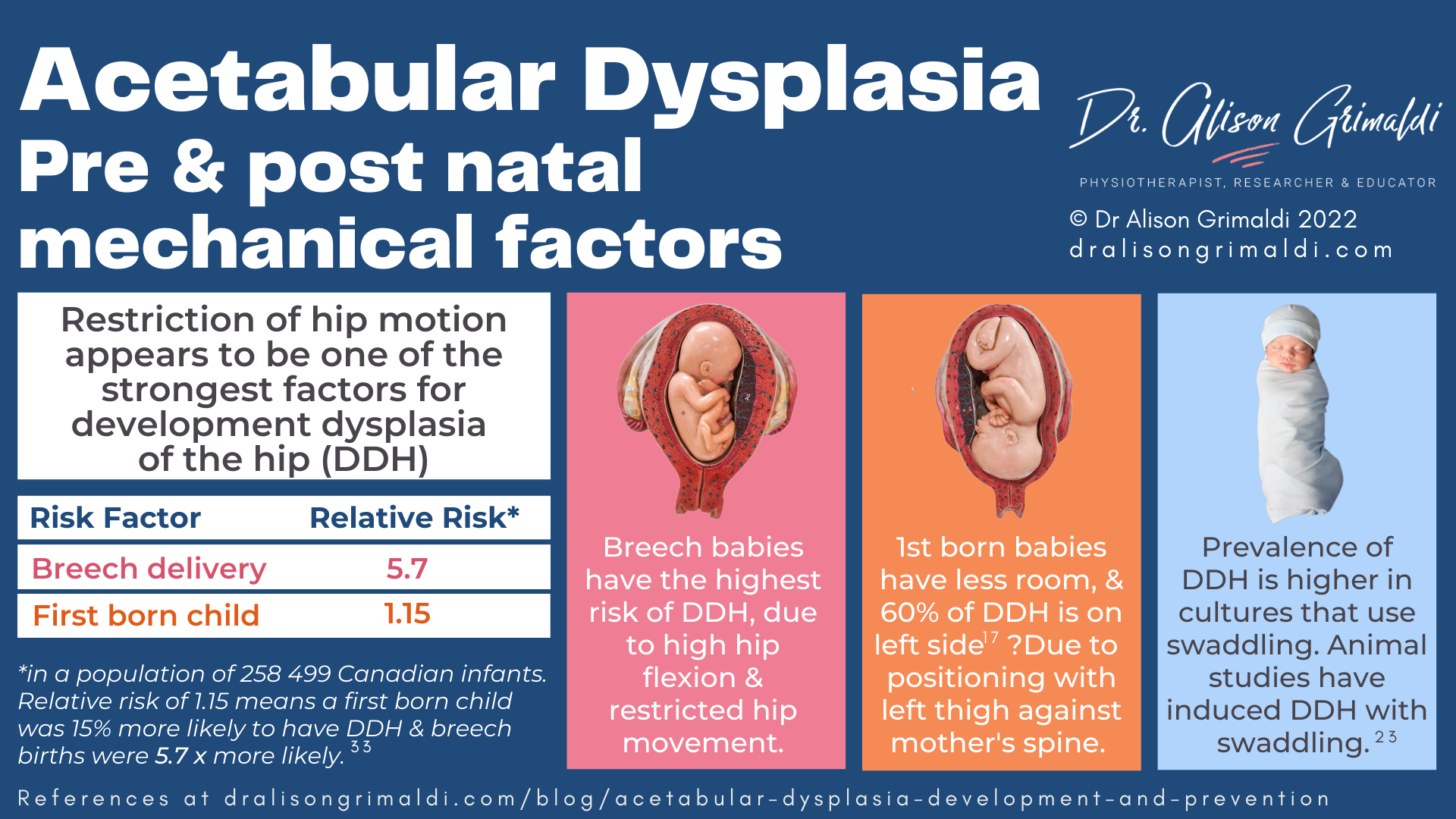
The aetiology of acetabular dysplasia is often multifactorial, with most factors imposing their effect in utero, resulting in developmental dysplasia of the hip (DDH). Common factors include breech positioning in utero, family history, female sex and being the first-born child.16
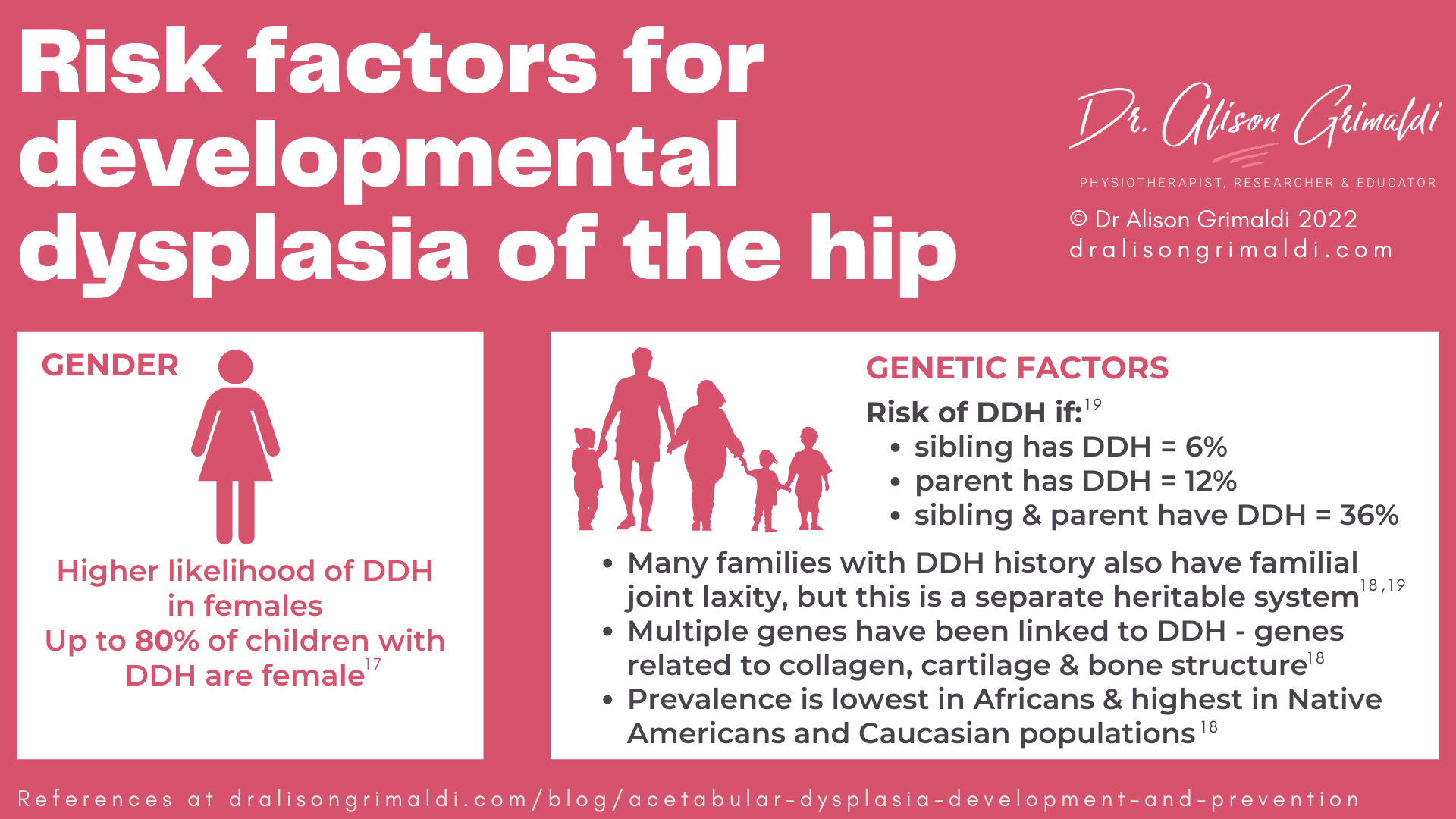
Sex differences
Risk of developmental dysplasia is much higher in females, with up to 80% of affected children being female. This is hypothesized to be associated with higher ligamentous laxity and therefore greater hip flexion in utero (see information of mechanical loading below).17 But other factors such as family history and being first born may amplify that risk.
Genetic factors
While there is not a single gene for acetabular dysplasia or developmental dysplasia of the hip, scientists have identified different chromosome loci that are associated with DDH. These are primarily genes involved with structure of connective tissues, osteo- and chondrogenesis (genes involved in formation of bone and cartilage), and formation of joints.18
Harsanyi et al (2020) reported that family history and genetic factors increase risk of DDH twelvefold in first degree relatives.18 An early study of 589 patients and their families found that if a child has a sibling with DDH, the risk is 6%, if the parent had DDH, the risk increases to 12% and if both a parent and a sibling had DDH, the risk jumps to 36%.19
Many of these families also had familial joint laxity, but their research found that acetabular dysplasia is a separate heritable system in some families. So for some, the genes involved may be the same genes related to expression of a hypermobility spectrum disorder, but hypermobility is not present in all families with acetabular dysplasia.19
There are also variations in prevalence across different ethnicities, with prevalence lowest in Africans, and highest in Native Americans and Caucasian populations.18
The influence of mechanical loading on development of the acetabulum
Mechanical loading in utero
In last month’s blog, we discussed how the levering of the femur against the Anterior Superior Iliac Spine (ASIS) results in femoral anteversion in utero. That same mechanism influences the development of the acetabulum.20
Approximation of the femoral head is one of the key stimuli for formation of the acetabulum, the socket forming around the femoral head. If the hips are hyperflexed in utero and the femoral head is levered further away from the pelvis, the acetabulum will be relatively more shallow at birth. Interestingly, large apes that have a flat ilium without prominent iliac spines, do not develop dysplasia. 20
The higher risk of developmental dysplasia in breech births, first born babies and in cases of oligohydramnios (low amniotic fluid) has been linked to this hyperflexion mechanism, due to reduced space in utero.
Breech birth appears to be the strongest single factor for the development of acetabular dysplasia, with delivery method having no effect i.e., a caesarean birth is not protective. This means it is the sustained breech positioning in utero and not the process of a natural breech delivery that impacts on the acetabulum.21
The link with ligamentous laxity may also be two-fold, firstly genetic predisposition and secondly, in a hyperflexed hip position, the more extensible hip capsule and ligaments will result in less approximation and moulding of the acetabulum by the femoral head.
Mechanical loading in utero also appears to have a side-effect, with 60% of cases of DDH being left sided, 20% right sided and 20% bilateral. The hypothesis here is that this distribution is related to the most common position in utero where the baby is head down, facing backwards but on an angle, so that the baby’s left thigh is against the mother’s spine with less room to abduct.17
Verbruggen and co-authors (2018) also found kick forces in utero are reduced in breech positioning, oligohydramnios and first-born babies, linking biomechanics of foetal movements and risk factors of acetabular dysplasia.22
Swaddling and acetabular dysplasia
What we do with our baby’s hips in the post-natal period, can also have a marked impact on acetabular development. An abducted hip position is important to create a medialising force, where ligaments and muscles approximate the femoral head and encourage the acetabulum to mould around it.
In populations that practice tight swaddling, with the hips sustained in an extended, adducted hip position, prevalence of acetabular dysplasia is higher.16 An animal model also demonstrated that straight-leg swaddling of immature rats significantly increased the prevalence of acetabular dysplasia and associated hip subluxation or dislocation, particularly if the swaddling was early or prolonged.23
The influence of the proximal femur on development of acetabular shape
Femoral neck shaft angle and femoral head shape (and presence) are tightly linked with the development of the acetabulum.
Neck-shaft angle has been shown to correlate with acetabular volume in immature sheep on which femoral osteotomies were performed to study influence on acetabular development.24 The lower the neck-shaft angle, the higher the acetabular volume. Coxa valga, a more vertical femoral neck was therefore associated with relatively lower acetabular volume.
Femoral neck-shaft angle typically reduces over childhood, secondary to the gravitational and muscle forces associated with upright function.25 This increasing neck shaft angle will then contribute to developing further depth in the acetabulum.
Those with acetabular dysplasia are more likely to have coxa valga - a higher neck-shaft angle (more vertically oriented neck).26 Those with coxa vara (low femoral neck-shaft angle) may also have acetabular dysplasia, but it would appear this is most likely also in association with other proximal femoral deformities like an aspherical femoral head and shortening of the femoral neck which may influence abductor forces (read more on abductor forces below).
The influence of muscle forces on development of acetabular shape
The primary influence of muscle forces on acetabular development is likely to be mediated by forces imposed on the proximal femur.
In a modelling study of the influence of hip muscle forces during gait, Yadav and colleagues (2017), found that hip abductor force contributes to proximal femoral growth more than any other muscle group.27 The effect of hip abductor muscle forces in gait is to induce reduction of femoral neck-shaft angle while the growth plates are open.27 Lower neck-shaft angles then help to mould a deeper acetabulum.
A recent study aimed to examine the influence of muscle tone on development on proximal femoral and acetabular geometry.28High adductor tone in cerebral palsy (CP) has long been hypothesized to be one of the major factors contributing to hip displacement in this population, although adductor tenotomy and botox have been shown to have inadequate influence.
Ulusaloglu and colleagues (2022) compared sequential hip radiographs collected over the first 6-8 years of life in children with CP (spastic type – high muscle tone) and spinal muscular atrophy (SMA - low muscle tone) who developed hip displacement.28
Neck-shaft angle and acetabular index (roof angle) remained high in both groups from age 1 to 8 years, with hip displacement related to acetabular index but not muscle tone. The authors concluded that: ‘Abnormal physeal alignment may be causally related to weakness of the hip abductor muscles rather than spasticity or muscle imbalance, resulting in coxa valga and secondary acetabular dysplasia.’28
With respect to muscle forces, the hip abductors appear to be most likely to contribute to positive development of the proximal femur and acetabulum.
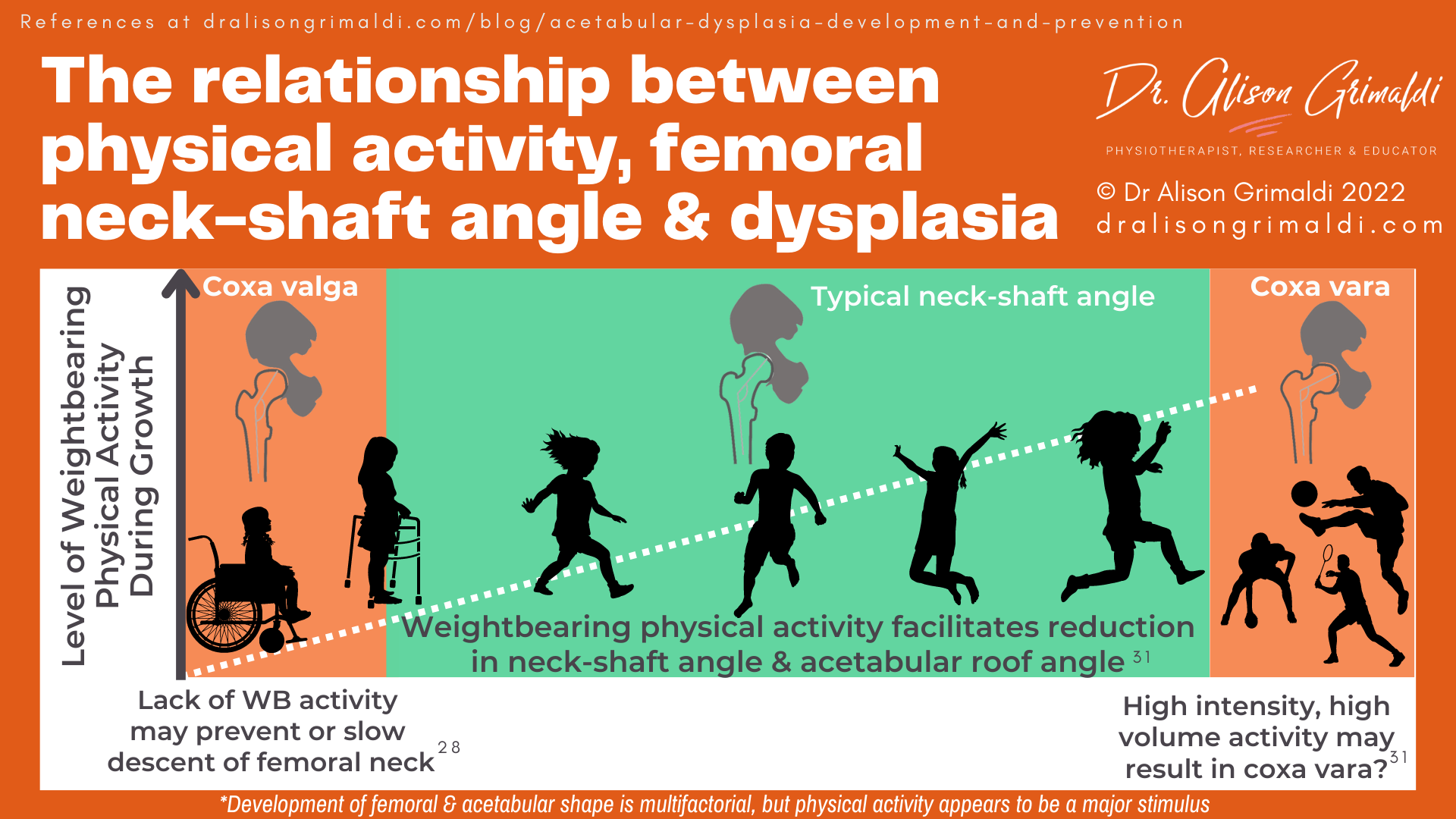
The influence of weightbearing and activity
The lack of change in neck-shaft angle and acetabular index (roof angle) reported by Ulusaloglu et al (2022) in children with CP and SMA is also likely to be inherently linked to lack of weightbearing function.28 These children had low levels of functional mobility, with the CP children classified as Level 4 and 5 on the Gross Motor Function Classification System (GMFCS) – mainly or always in a wheelchair.
Without normal weightbearing stimulus, neither group displayed the typical reductions in femoral neck-shaft angle and acetabular index, and therefore the acetabular development expected during growth.28
Others have also established a linear relationship between level of functional mobility (GMFCS level) and coxa valga (high neck-shaft angle) and hip displacement (femoral head migration) - the lower the functional mobility level, the higher the neck-shaft angle and greater the displacement of the femoral head.29,30
In children without neuromuscular disorders, physical activity is also a key stimulus for development of the proximal femur and subsequently the acetabulum. Yadav and colleagues (2021) used finite element modelling to predict growth rate and growth direction of the proximal femur in response to various hip contact force scenarios walking, running, cycling, jumping.31 All of these common activities encourage natural reduction of the femoral neck-shaft angle with growth. Naturally, weightbearing activities have a dominant inferiorly oriented vector that helps lower the femoral neck-shaft angle over time.31
Prevention of Acetabular Dysplasia
Addressing risk factors for acetabular dysplasia
Most risk factors for acetabular dysplasia are non-modifiable – family/genetic factors, female sex, and being the first-born child. However, breech birth appears to be the strongest single factor and something that is potentially modifiable.
Verbruggen and coauthors suggest that earlier intervention to correct breech position through external cephalic version could reduce the risk of acetabular dysplasia.22 This involves the obstetrician trying to turn the baby into a head-down position by applying pressure on the abdomen. This is unlikely to be suitable or successful for all cases but is something to consider.
Screening for developmental dysplasia of the hip
Introduction of neonatal screening in Australia in 1964 had a substantial impact on late presentation of DDH at walking age, reducing from 1.2/1000 in 1960-64 to 0.2/1000 in 1970-73.32 Clinical and/or sonographic screening of newborns has generally decreased the incidence of late presentation and requirement for surgery at a later age.33
However, a more recent study in South Australia (2016) reported an increase in late diagnosed cases with DDH despite implementation of a clinical screening program.34 The link between breech births and developmental dysplasia of the hip is fairly well recognised now, and breech babies with DDH are most likely to be identified early.34
First-born babies and those with a family history are also more likely to be closely screened, and sent for an ultrasound check, but DDH in second-born babies and non-breech presentations may be missed. Studer and colleagues called for greater awareness in health professionals performing screening, outside the high-risk groups.
An increase in the number of late DDH diagnoses has also been reported in the United Kingdom, North America and France over the last 10 years. Factors such as reduced clinical expertise in hip examination, lack of repeated hip checks of children until walking age, and a resurgence of swaddling practices as a technique for settling babies have been suggested as potential factors.34

Safe swaddling and baby carriers to prevent acetabular dysplasia
Even with a negative neonatal screening in hospital, dysplasia may present later associated with post-natal swaddling techniques, where the hips are held firmly in extension and adduction. Increasing awareness of dysplasia and education around moving from traditional swaddling to ‘safe swaddling’ where the legs are provided room to freely move into flexion-abduction, can have a marked effect of prevalence of dysplasia.
In a study of Native Americans, prevalence dropped from 6 times the United states average to the same as the rest of the country with a change in swaddling practices.17 In Japan, a public education campaign to eliminate swaddling and introduction of a clinical screening program reduced the incidence of DDH from 5-6% to less than 0.4%.35
Graham and colleagues (2015) reviewed hospital records over 16 years in Malawi and found that no infant presented with, or underwent surgical intervention, for symptomatic DDH.36 They suggested an important factor in the lack of DDH in this population may be the fact that most babies are carried on the mother’s back during the first 2 to 24 months of life, with their hips in a flexed-abducted position, similar to a Pavlik harness. Baby carriers that allow hip flexion-abduction are a great option for healthy hips.
Early intervention to prevent adult acetabular dysplasia
When DDH is detected early, outcomes are generally very good, which is why screening remains one of the best weapons we have against late presentation DDH and adult dysplasia.
The Pavlik harness that holds the hips in a flexed-abducted position, remains the primary treatment for the younger infant with DDH. Those that fail to achieve stability with the Pavlik harness may go on to closed reduction and spica casting. Children older than 18 months with persistent DDH may require surgical intervention.17
To reduce prevalence of acetabular dysplasia, a condition that has such a potent adverse impact on hip health, health professionals can:
- play a role in performing or promoting neonatal screening for developmental dysplasia of the hip,
- be aware of high-risk groups (breech, family history, female, first-born), but ensure screening is provided for all,
- contribute to public education around the condition and infant hip positioning:
- avoid traditional swaddling in hip extension-adduction
- swap to ‘safe swaddling’ where the legs are free to flex and abduct
- encourage baby carriers that position the hips in flexion-abduction
- encourage some ‘tummy time’, where the hips are generally forced into abduction,
- encourage weightbearing physical activity in children, and
- optimise hip muscle function (particularly the abductors) in children and early adolescents where there may be concerns around hip stability and acetabular dysplasia.
You can find heaps more information about assessing hip stability and managing joint related pain associated with acetabular dysplasia in the courses and technique videos available within Hip Academy.
-
- A detailed examination of mechanisms of physical overload (morphology, movement, muscle) and impairments associated with anterior hip pain and groin pain, clinical diagnostic tests and management approaches.
- Including joint related-pain & bony impingement (intra & extra-articular), soft tissue-related pain and nerve-related pain.

- All Online Hip Courses
- eBook Series
- Growing How-to Video Library
- Growing PDF Resource Library
- Live Hip Academy Zoom Meetings - Additional exclusive lecture content
- Recordings of all previous meetings
- Hip Academy Forum
Check Out Some More Relevant Blogs
Another great Anterior Hip Pain blog

Anterior Hip Pain: Causes & Contributing Factors
Adequate consideration of individual causes and contributing factors is important for best outcomes.
References
- Wilkin G, Ibrahim M, Smit K and Beaulé P. A Contemporary definition of hip dysplasia and structural instability: Toward a comprehensive classification for acetabular dysplasia. The Journal of Arthroplasty. 2017;32(9):S20-S27.
- Ruiz Santiago F, Santiago Chinchilla A, Ansari A, Guzmán Álvarez L, Castellano García Mdel M, Martínez Martínez A, Tercedor Sánchez J. Imaging of hip pain: From radiography to cross-sectional imaging techniques. Radiol Res Pract. 2016;2016:6369237.
- Mannava S, Geeslin AG, Frangiamore SJ, Cinque ME, Geeslin MG, Chahla J, Philippon MJ. Comprehensive clinical evaluation of Femoroacetabular Impingement: Part 2, Plain Radiography. Arthrosc Tech. 2017 Oct 30;6(5):e2003-e2009.
- Tannast M, Hanke MS, Zheng G, Steppacher SD, Siebenrock KA. What are the radiographic reference values for acetabular under- and overcoverage? Clin Orthop Relat Res. 2015 Apr;473(4):1234-46.
- Siebenrock KA, Kistler L, Schwab JM, Büchler L, Tannast M. The acetabular wall index for assessing anteroposterior femoral head coverage in symptomatic patients. Clin Orthop Relat Res. 2012 Dec;470(12):3355-60.
- Gala L, Clohisy JC, Beaulé PE. Hip Dysplasia in the Young Adult. J Bone Joint Surg Am. 2016 Jan 6;98(1):63-73.
- Song K, Pascual-Garrido C, Clohisy JC, Harris MD. Acetabular edge loading during gait is elevated by the anatomical deformities of hip dysplasia. Front Sports Act Living. 2021 Jul 1;3:687419.
- Song K, Pascual-Garrido C, Clohisy JC, Harris MD. Elevated loading at the posterior acetabular edge of dysplastic hips during double-legged squat. J Orthop Res. 2022 Sep;40(9):2147-2155.
- Henak CR, Ellis BJ, Harris MD, Anderson AE, Peters CL, Weiss JA. Role of the acetabular labrum in load support across the hip joint. J Biomech. 2011 Aug 11;44(12):2201-6.
- Jacobsen JS, Jakobsen SS, Søballe K, Hölmich P, Thorborg K. Isometric hip strength impairments in patients with hip dysplasia are improved but not normalized 1 year after periacetabular osteotomy: a cohort study of 82 patients. Acta Orthop. 2021 Jun;92(3):285-291.
- Jacobsen JS, Hölmich P, Thorborg K, Bolvig L, Jakobsen SS, Søballe K, Mechlenburg I. Muscle-tendon-related pain in 100 patients with hip dysplasia: prevalence and associations with self-reported hip disability and muscle strength. J Hip Preserv Surg. 2017 Nov 17;5(1):39-46.
- Lee MC, Eberson CP. Growth and development of the child's hip. Orthop Clin North Am. 2006 Apr;37(2):119-32.
- Hingsammer AM, Bixby S, Zurakowski D, Yen YM, Kim YJ. How do acetabular version and femoral head coverage change with skeletal maturity? Clin Orthop Relat Res. 2015 Apr;473(4):1224-33.
- Fabricant PD, Hirsch BP, Holmes I, Kelly BT, Lorich DG, Helfet DL, Bogner EA, Green DW. A radiographic study of the ossification of the posterior wall of the acetabulum: implications for the diagnosis of pediatric and adolescent hip disorders. J Bone Joint Surg Am. 2013 Feb 6;95(3):230-6.
- Monazzam S, Bomar JD, Dwek JR, Hosalkar HS, Pennock AT. Development and prevalence of femoroacetabular impingement-associated morphology in a paediatric and adolescent population: a CT study of 225 patients. Bone Joint J. 2013 May;95-B(5):598-604.
- Yang S, Zusman N, Lieberman E, Goldstein RY. Developmental Dysplasia of the Hip. Pediatrics. 2019 Jan;143(1):e20181147.
- Kotlarsky P, Haber R, Bialik V, Eidelman M. Developmental dysplasia of the hip: What has changed in the last 20 years? World J Orthop. 2015 Dec 18;6(11):886-901.
- Harsanyi S, Zamborsky R, Krajciova L, Kokavec M, Danisovic L. Developmental Dysplasia of the Hip: A Review of Etiopathogenesis, Risk Factors, and Genetic Aspects. Medicina (Kaunas). 2020 Mar 31;56(4):153.
- Wynne-Davies R. Acetabular dysplasia and familial joint laxity: two etiological factors in congenital dislocation of the hip. A review of 589 patients and their families. J Bone Joint Surg Br. 1970 Nov;52(4):704-16.
- Hogervorst T, Eilander W, Fikkers JT, Meulenbelt I. Hip ontogenesis: how evolution, genes, and load history shape hip morphotype and cartilotype. Clin Orthop Relat Res. 2012 Dec;470(12):3284-96.
- de Hundt M, Vlemmix F, Bais JM, Hutton EK, de Groot CJ, Mol BW, Kok M. Risk factors for developmental dysplasia of the hip: a meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2012 Nov;165(1):8-17.
- Verbruggen SW, Kainz B, Shelmerdine SC, Arthurs OJ, Hajnal JV, Rutherford MA, Phillips ATM, Nowlan NC. Altered biomechanical stimulation of the developing hip joint in presence of hip dysplasia risk factors. J Biomech. 2018 Sep 10;78:1-9.
- Wang E, Liu T, Li J, Edmonds EW, Zhao Q, Zhang L, Zhao X, Wang K. Does swaddling influence developmental dysplasia of the hip? An experimental study of the traditional straight-leg swaddling model in neonatal rats. J Bone Joint Surg Am. 2012 Jun 20;94(12):1071-7.
- Moraleda L, Bravo C, Forriol F, Albiñana J. Does Orientation of the Femoral Head Affect Acetabular Development? An Experimental Study in Lamb. J Pediatr Orthop. 2019 Sep;39(8):416-421.
- Djurić M, Milovanović P, Djonić D, Minić A, Hahn M. Morphological characteristics of the developing proximal femur: a biomechanical perspective. Srp Arh Celok Lek. 2012 Nov-Dec;140(11-12):738-45.
- Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009 Jan;467(1):128-34.
- Yadav P, Shefelbine SJ, Pontén E, Gutierrez-Farewik EM. Influence of muscle groups' activation on proximal femoral growth tendency. Biomech Model Mechanobiol. 2017 Dec;16(6):1869-1883.
- Ulusaloglu AC, Asma A, Rogers KJ, Shrader MW, Graham HK, Howard JJ. The influence of tone on proximal femoral and acetabular geometry in neuromuscular hip displacement: A comparison of cerebral palsy and spinal muscular atrophy. J Child Orthop. 2022 Apr;16(2):121-127.
- Soo B, Howard JJ, Boyd RN, et al. Hip displacement in cerebral palsy. J Bone Joint Surg Am 2006; 88: 121–129.
- Robin J, Graham HK, Selber P, et al. Proximal femoral geometry in cerebral palsy: a population-based cross-sectional study. J Bone Joint Surg Br 2008; 90(10): 1372–1379.
- Yadav P, Fernández MP, Gutierrez-Farewik EM. Influence of loading direction due to physical activity on proximal femoral growth tendency. Med Eng Phys. 2021 Apr;90:83-91.
- Paterson D. Early diagnosis and treatment of congenital dislocation of the hip. Aust N Z J Surg 1976;46:359-66.
- Pollet V, Percy V, Prior HJ. Relative Risk and Incidence for Developmental Dysplasia of the Hip. J Pediatr. 2017 Feb;181:202-207.
- Studer K, Williams N, Antoniou G, Gibson C, Scott H, Scheil WK, Foster BK, Cundy PJ. Increase in late diagnosed developmental dysplasia of the hip in South Australia: risk factors, proposed solutions. Med J Aust. 2016 Apr 4;204(6):240: e1-6.
- Yamamuro T, Ishida K. Recent advances in the prevention, early diagnosis, and treatment of congenital dislocation of the hip in Japan. Clin Orthop Relat Res 1984; (184): 34-40.
- Graham SM, Manara J, Chokotho L, Harrison WJ. Back-carrying infants to prevent developmental hip dysplasia and its sequelae: is a new public health initiative needed? J Pediatr Orthop. 2015 Jan;35(1):57-61.