Surgical Management of Hip Osteoarthritis – Types of Prostheses and Approaches
Includes videocast, podcast, infographic & video/podcast notes. When the time does come for surgery for advanced hip osteoarthritis, it's not one size fits all in terms of surgical and prosthetic options. There are choices around conventional Total Hip Replacement or Hip Resurfacing, cemented or uncemented prostheses, bearing surfaces and surgical approaches to the hip. This interview presented in both videocast and podcast format, explores the options available and the relative indications, advantages and disadvantages, limitations or risks. It is important for non-surgical health professionals to be aware of these options as there are implications for post-operative management and advice provided to patients undergoing or who have undergone various surgical procedures for advanced hip osteoarthritis.
Watch the interview here:
or if you prefer, listen to the interview here (Podcast only):
About Associate Professor Patrick Weinrauch :
Associate Professor Patrick Weinrauch is an Orthopaedic Surgeon, founder of Brisbane Hip Clinic in Queensland, Australia. The name of his clinic says it all. He focuses exclusively on the management of hip joint disorders, with a high level of experience and expertise in a full range of surgical procedures for the hip, including hip joint arthroscopy, hip joint preservation surgery, hip resurfacing and hip replacement procedures. Dr Weinrauch is a Fellow of the Royal Australasian College of Surgeons and a Fellow of the Australian Orthopaedic Association, and not only has a busy clinical practice but contributes to education programs for other surgeons and health professionals and to scientific research in this field. Dr Weinrauch has published over 50 peer-reviewed scientific papers and is the Deputy Editor for the International Journal of Advanced Joint Reconstruction. He is currently appointed as an Associate Professor at the Griffith University School of Medicine and has been awarded a Doctorate of Philosophy and Master of Engineering for his research relating to the surgical management of adult hip joint disorders. We are very grateful to Patrick for sharing his valuable time and wisdom.
Video/Podcast Notes
The decision about going to surgery and which implant are blended.
So the first question is, ‘Do I need a joint replacement?’ based on function, pain, response to other therapies, degree of osteoarthritic wear.
If the answer to the first question is ‘Yes’, then the next question is ‘Which implant is the suitable one for me?’
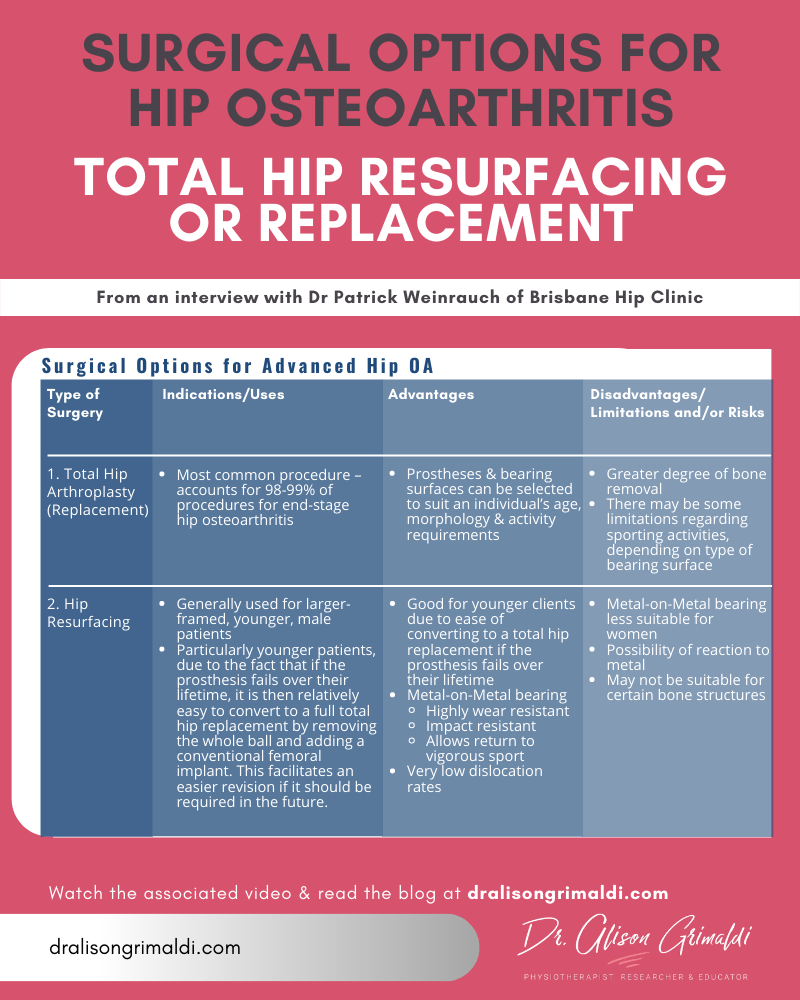
Surgical Options for Total Hip Replacement
The two main surgical options:
1. Conventional Total Hip Replacement
• Most common procedure – 98-99% of procedures for hip osteoarthritis
2. Hip Resurfacing
• For select scenarios
For appropriately selected patients who meet the criteria for those implants, the expectation is for a consistently good long-term outcome, with complete or near complete pain relief.
Prostheses for Total Hip Replacement
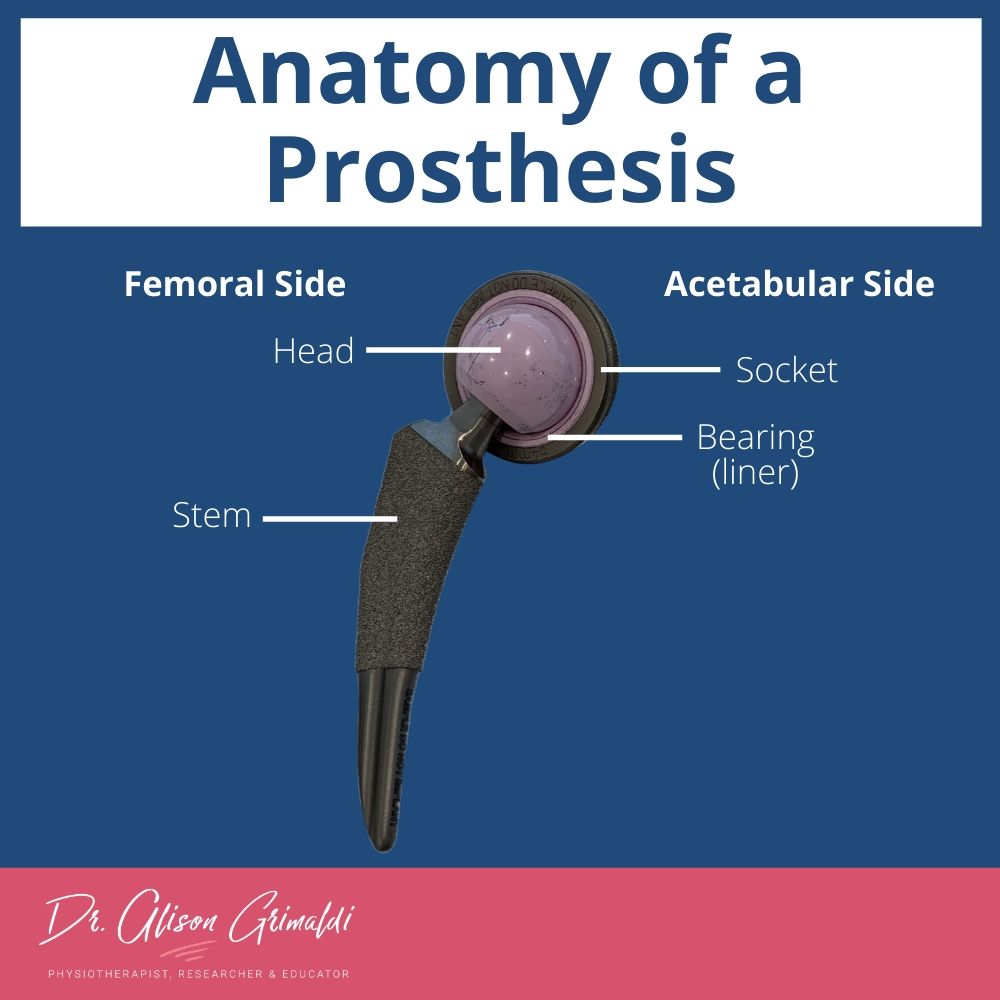
‘Anatomy’ of a Hip Prosthesis
• Femoral side - consists of a stem and a head component
• Acetabular side – socket with a bearing inside - the liner
Two main categories of Total Hip Replacement
1. Cemented
• Uses some form of grout to bond the implant to the bone
2. Uncemented
• No grout used, bone will grow directly onto the implant
The femoral stem of an uncemented prosthesis
• Generally made of titanium
• The stem is coated with a spray, either of titanium or a calcium spray called hydroxyapatite, to stimulate bone to grow directly onto the stem – this creates a very firm bond of the prosthesis within the femur
• Titanium is a well-tolerated metal, which is not associated with allergy and bonds very well with bone.
• While titanium is excellent as stem material, it is a relatively soft metal and is therefore not good as a bearing surface, so other materials are used for the bearing surfaces of the ball and socket
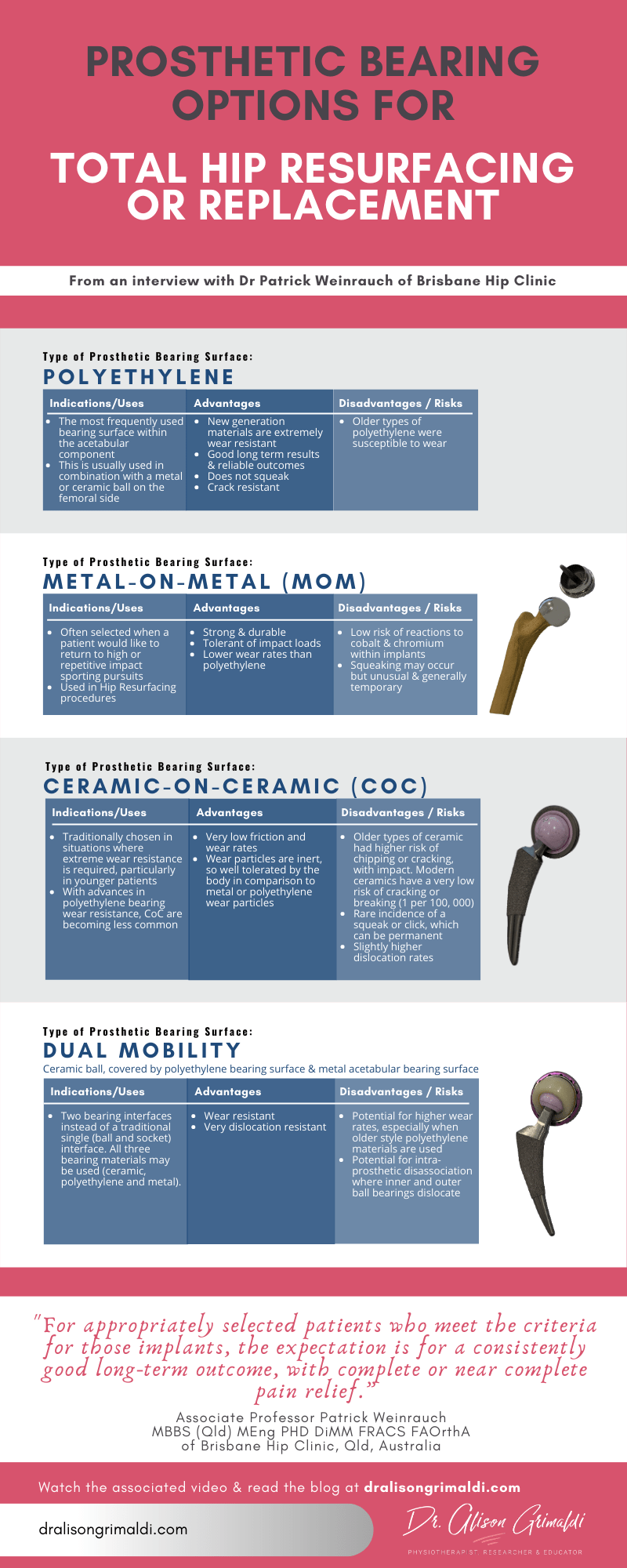
Bearing surface options for Total Hip Replacement or Hip Resurfacing
The femoral component of a hip prothesis
• Polyethylene
i. A plastic-like material
ii. Has changed a lot over the last 20 years – now highly-linked polyethylene is used, where all the fibres are linked together and the molecular structure is very long
iii. Current day polyethylene is therefore extremely wear-resistant
iv. Vast majority of protheses now have some polyethylene component
• Ceramic
i. May be used alone as the bearing surface of the femoral head, or in combination with a second bearing surface
ii. Advantages of ceramic surface is that they are very smooth, and when they are wet by the synovial fluid, they are extremely slippery, so the wear rate is very low.
• Combination – The Dual Mobility Implant
i. Ceramic inner ball
ii. Combined with an outer ball - a second bearing surface over the top made of polyethylene, which rotates freely over the inner ball
The acetabular component of a hip prosthesis
• Socket implant is often made of 2 parts
i. Titanium shell that the bone can grow onto it
ii. Bearing surface that lines the shell and communicates with the femoral head
• Types of bearing surface
i. Ceramic bearing surface, so that a Ceramic-on-Ceramic implant refers to an implant where the bearing surface of both the ball and the socket are both made of ceramic
ii. Polyethylene
iii. Cobalt Alloy – wear resistant metal. This is used in the Dual Mobility Implant, so that the polyethylene outer ball sits over the ceramic ball and articulates with the Cobalt Alloy bearing surface of the socket.
Hip Resurfacing
• Is a bone preserving alternative to conventional hip replacement – the bone is preserved and only the damaged cartilage is replaced
• Is still a prosthetic joint replacement with the same recovery and rehabilitation periods and requirements.
• Is not a lesser operation, just a different implant
Process
• Instead of removing the head and placing a stem down the femur, the procedure involves shaving around the outside of the ball and placing a hollow metal cap over the ball
• The socket is also shaved out and lined with a metal liner
Criteria for suitability for Hip Resurfacing
• Are very stringent
• Generally used for larger-framed, male patients
• Particularly younger patients, due to the fact that if the prosthesis fails over their lifetime, it is then relatively easy to convert then to a full total hip replacement by removing the whole ball and adding a conventional femoral implant. This facilitates an easier revision if it should be required in the future.
Prosthetic Failure in Total Hip Replacement or Hip Resurfacing
Two main causes:
1. Aseptic loosening
- the most common form of failure of an implant
- related to wearing of the bearing surface – usually the polyethylene component, and impact of the debri on the bond between the implant and the bone
- rates of loosening are likely to reduce over time due to the use of far more wear-resistant bearings of modern implants
- can have loosening of either femoral or acetabular component
- revision surgery may involve replacement of either the ball or socket or both components, depending on the situation
2. Instability associated with dislocation
- 2nd most likely cause of revision in Australia
- A revision is not always necessary following dislocation, but recurrent dislocation is an indication for revision surgery
- May develop over longer periods of time related to changes in posture, pelvic position and relative loads across the joint that may change with ageing – this situation may only require a reorientation of the socket component.
- Revision of modern modular implants
• Modern implants are modular, comprised of a number of connecting components. This gives the surgeon lots of options to choose components that are most suited to the individual’s requirements and morphology
• This also means that if one component fails, the whole implant does not necessarily need to be replaced. For example, if the femoral head fails, it can be removed easily from the stem and replaced with another ball, without needing to replace the stem component
• If a well fixed stem does need to be replaced, this involves a larger surgical procedure, usually with a longer rehabilitation time post-operatively.
Selection of Prosthesis in Total Hip Replacement or Hip Resurfacing
Joint replacement technologies and implants are not a one-size-fits all scenario.
Determined by:
1. Surgeon Preference
• Associated with experience, reading of the literature, familiarity with different implant designs
• Implants that have a good track record with the particular application
2. Patient Criteria
• Bone density
• Bone shape
• Leg length
• Muscle length-tension relationships
• Age
• Anticipated activity requirements – nature and volume of activities
Considerations for a younger patient:
• May be a candidate for a bone preserving surgery such as hip resurfacing
• A stem with a shorter length or reducing area of porous coating may be selected, so that the stem is easier to remove in the future, if revision is required
Considerations for patients who would like to return to repetitive impact activities:
• Would choose implant designs that are more wear resistant and impact resistance
• Also, non-modular implants may be more appropriate, as each junction may be a source of failure under repetitive load situations
• Metal on metal implants such as that used in hip resurfacing are very wear resistant
• Previously there have been concerns regarding ceramic bearing surfaces in repetitive impact loading tasks and the potential risk of cracking or chipping of the implant. However, ceramics have undergone much development and the modern ceramic bearing surfaces are very impact and wear resistant. The fracture rate is now extremely low, approximately 1 in 10 000, so most surgeons are happy for patients with the newer ceramic prostheses to return to casual running and fitness activities.
• Some of the older style ceramics used in total hip replacement had a fracture rate more like 1-2% and therefore health professionals need to be careful with recommendations for running or impact activities in those that have had a ceramic implant in situ for some time.
• For the more extreme athlete, competing in ultramarathons and ironman events, there will be a risk analysis – the higher the exposure to repetitive impact, the greater the risk of potential failure of the implant. In such cases, a non-modular prosthesis or hip resurfacing will provide least risk of failure under such conditions.
• Advantages of resurfacing for the extreme athlete:
i. Hip resurfacing implants are non-modular
ii. have extreme wear resistance and
iii. if failure does occur, there is the option to convert to a conventional total hip replacement.
Considerations for patients who would like to return to large ROM activities, such as yoga:
• Would choose implant designs that are more appropriate for extremes of range of motion, with high dislocation resistance
i. The Dual Mobility Implant – large femoral head size and the dual bearing bearing surface of the femoral head, provide high levels of dislocation resistance
ii. Hip resurfacing implants are also very stable, with risk of dislocation from a posterior approach about 0.5%
iii. For those with extreme risk of dislocation or recurrent dislocations of current prosthesis, there is an option of ‘Constraint’ where the liner of the socket grips onto the femoral head
Surgical Approaches for Total Hip Replacement
The approaches are named relative to the approach to the femur, for example a surgical approach from the back of the femur is called a Posterior Approach and from the front of the femur is called an Anterior Approach. There are also some other variations such as an anterolateral approach or a transfemoral approach, which includes a trochanteric osteotomy. The two most common current approaches are Posterior and Anterior.
1. Posterior Approach
• Still most common approach in Australia, representing about 80% of joint replacements
• Advantages
i. Very reproducible operation with many different patient anatomical presentations
ii. Provides good access to the whole of the joint – important for more difficult situations with unusual bone shape or complex revisions
• Higher rates of dislocation than anterior approach total hip replacement, although comparable with a hip resurfacing procedure which is done through a posterior approach.
2. Anterior Approach
• Represents most of the remaining 20% of hip joint replacements
• More recently adopted in Australia in larger volumes, although the approach has been around for quite some time
• Advantages
i. More stable prosthesis with lower dislocation rate of 0.5% or less, compared with 3-4% with posterior approach. Risk of revision due to instability is substantially reduced with an anterior approach total hip replacement.
ii. Smaller incision with less dissection of muscles around the hip joint, so rehabilitation in the early phases might be a little better with less patient discomfort.
With modern physiotherapy and rehabilitation, both approaches do well with good outcomes in the longer term.
That concludes our interview series on non-surgical and surgical options for those with hip osteoarthritis, thanks to Dr Patrick Weinrauch, orthopaedic surgeon. His insights will have been valuable to you all, I'm sure. If you are not signed up to the www.dralisongrimaldi.com mailing list, sign up today to receive alerts for my monthly blogpost. Don’t forget to explore the dralisongrimaldi.com site where you’ll find a wealth of clinically applicable information on all things hip.
Learn more about
CONTEMPORARY DIAGNOSTIC & MANAGEMENT STRATEGIES FOR ANTERIOR HIP & GROIN PAIN, here
Another great Anterior Hip Pain blog

Anterior Hip Pain: Causes & Contributing Factors
Adequate consideration of individual causes and contributing factors is important for best outcomes.
Discover our Anterior Hip & Groin Pain Course
If you enjoyed this blog, you might like to take the online course on Anterior Hip & Groin Pain - 5 hours of guided online video content. Better your skills and understanding of the anterior hip and groin and become equipped with the knowledge to administer clinical diagnostic tests and management strategies.