Hip ROM Restrictions in FAIS – Relevance and Implications
This blog will cover the following topics:
- The relationship between hip range of motion and symptom severity in patients with FAIS
- Key Findings – Hip ROM and symptom severity in hip impingement
- Clinical relevance – what do these findings about hip ROM and FAIS symptoms mean for clinical practice
- Reasons for limited hip ROM in patients with FAIS and what to do about it
- Bony impingement and range restriction in FAIS
- Grumpy hips and protective patients – ROM limitation related to pain, effusion and self-protection
- Limitation of active hip flexion range related to hip flexor dysfunction TEST
The relationship between hip range of motion and symptom severity in patients with FAIS
Let’s take a look at what the study involved and what they found.
Gomes and colleagues (2025)1 analysed baseline data from 150 participants of the PhysioFIRST trial,2 all with cam-type FAIS (painful hip impingement related to an aspherical femoral head). So that you understand the population, mean age was around 35 years, around 50% were female and mean alpha angle was around 73° (measures the size of the cam).
Hip range of motion was assessed actively, with the contralateral thigh belted to the bed. Flexion was measured in supine and rotation in sitting with hips at 90° flexion. Symptom severity was gauged using the symptoms subscale of the international Hip Outcome Tool-33 (iHot-33), including questions on pain, stiffness and functional limitations. TEST
Key Findings – Hip ROM and symptom severity in hip impingement TEST
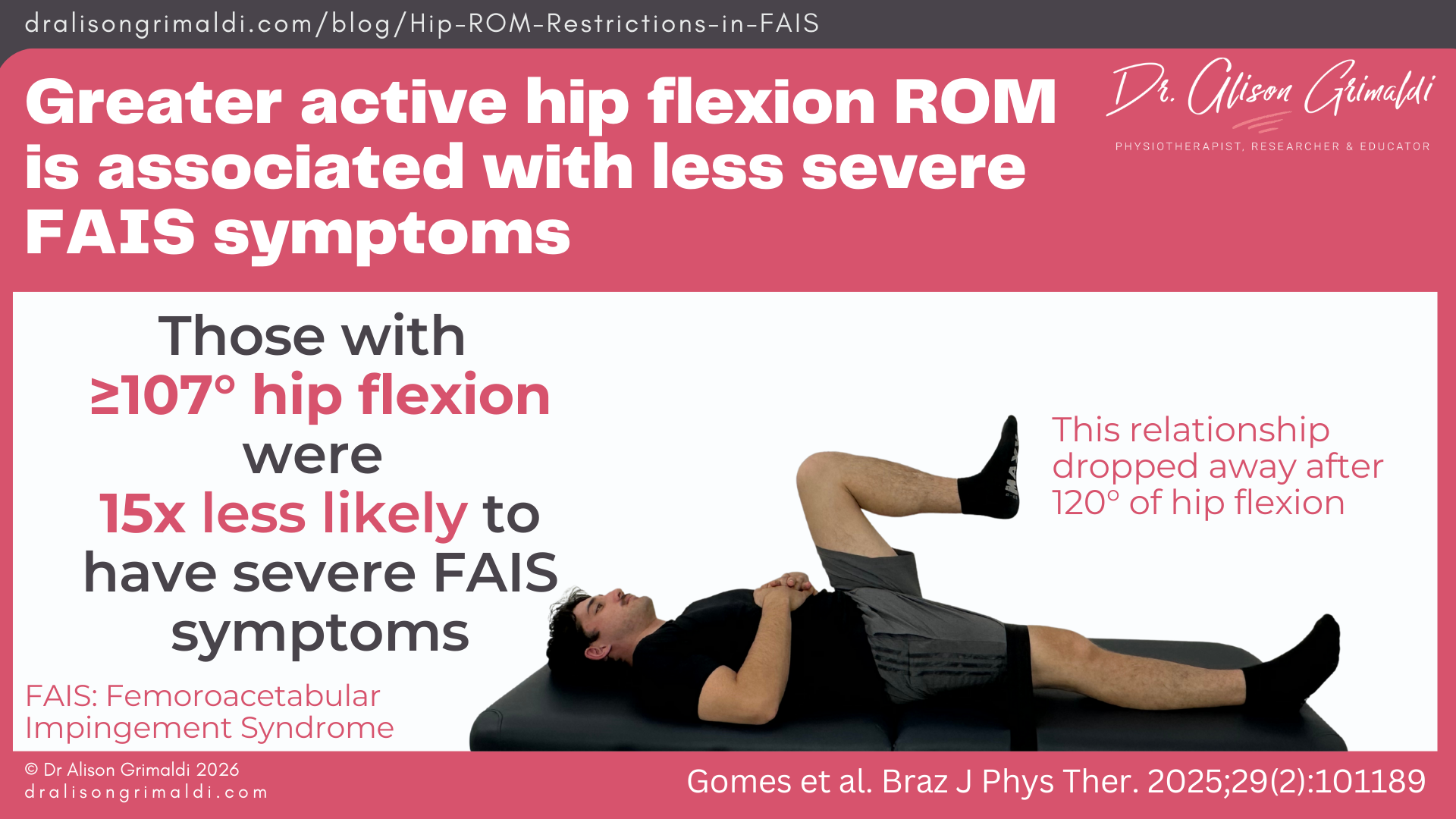
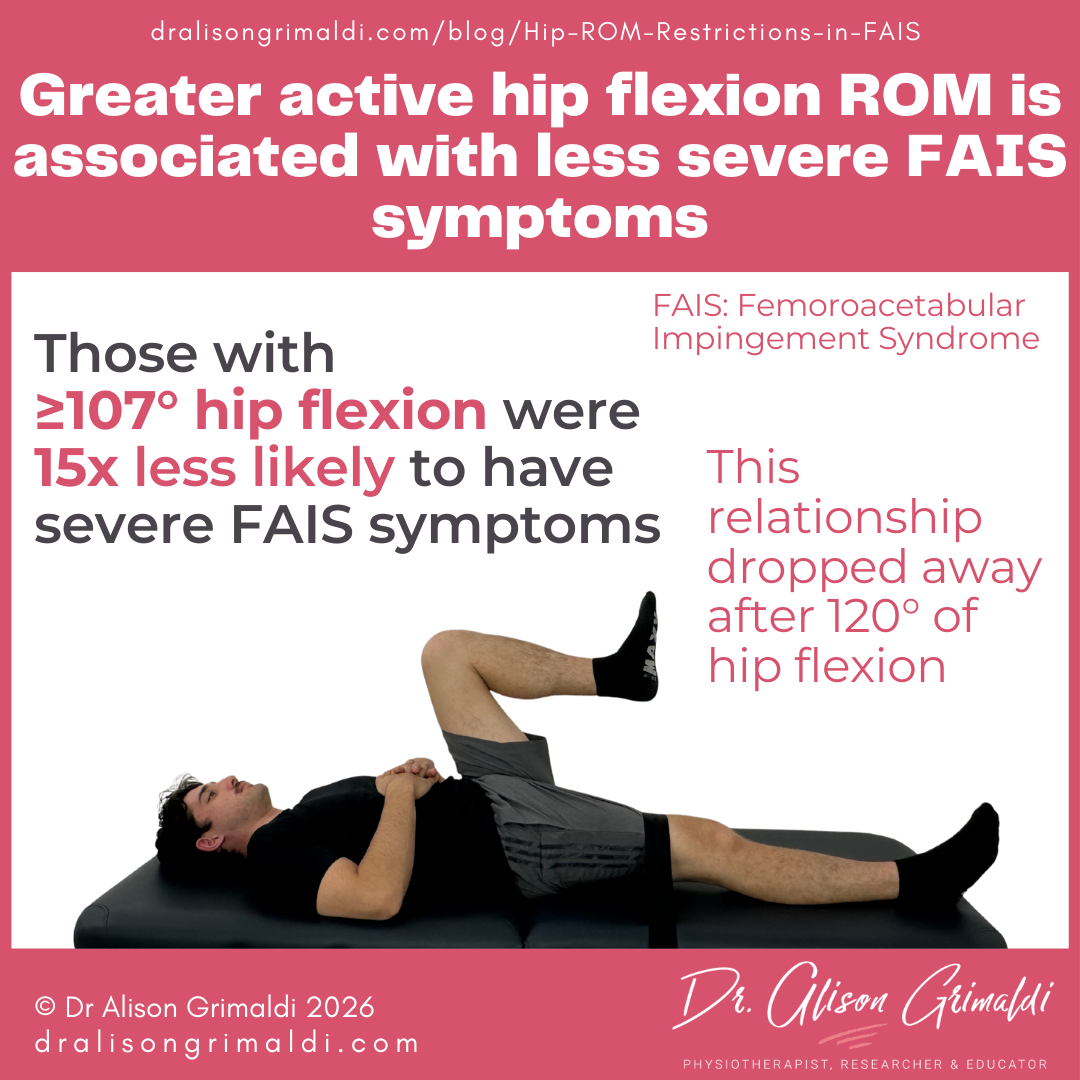
1. Greater active hip flexion ROM values are associated with less severe FAIS symptoms TEST
- Reduced hip flexion ROM appears to be an indicator of worse symptoms in FAIS.
- Reduced hip flexion ROM explained 24% of symptom variance in FAIS.
- Those with ≥107° of hip flexion were 15x less likely to have severe FAIS symptoms.
- The relationship between higher flexion ROM and better symptoms dropped off at around 120° flexion. TEST
2. Only a weak association existed between active hip internal rotation ROM and FAIS symptoms
- Active hip internal rotation ROM only explained 3% of the variance in FAIS symptoms, with questionable clinical relevance. TEST
3. Hip external rotation ROM was not associated with symptoms of FAIS
Clinical relevance – what do these findings about hip ROM and FAIS symptoms mean for clinical practice?
Hip flexion is a highly functional action, impacted by FAIS
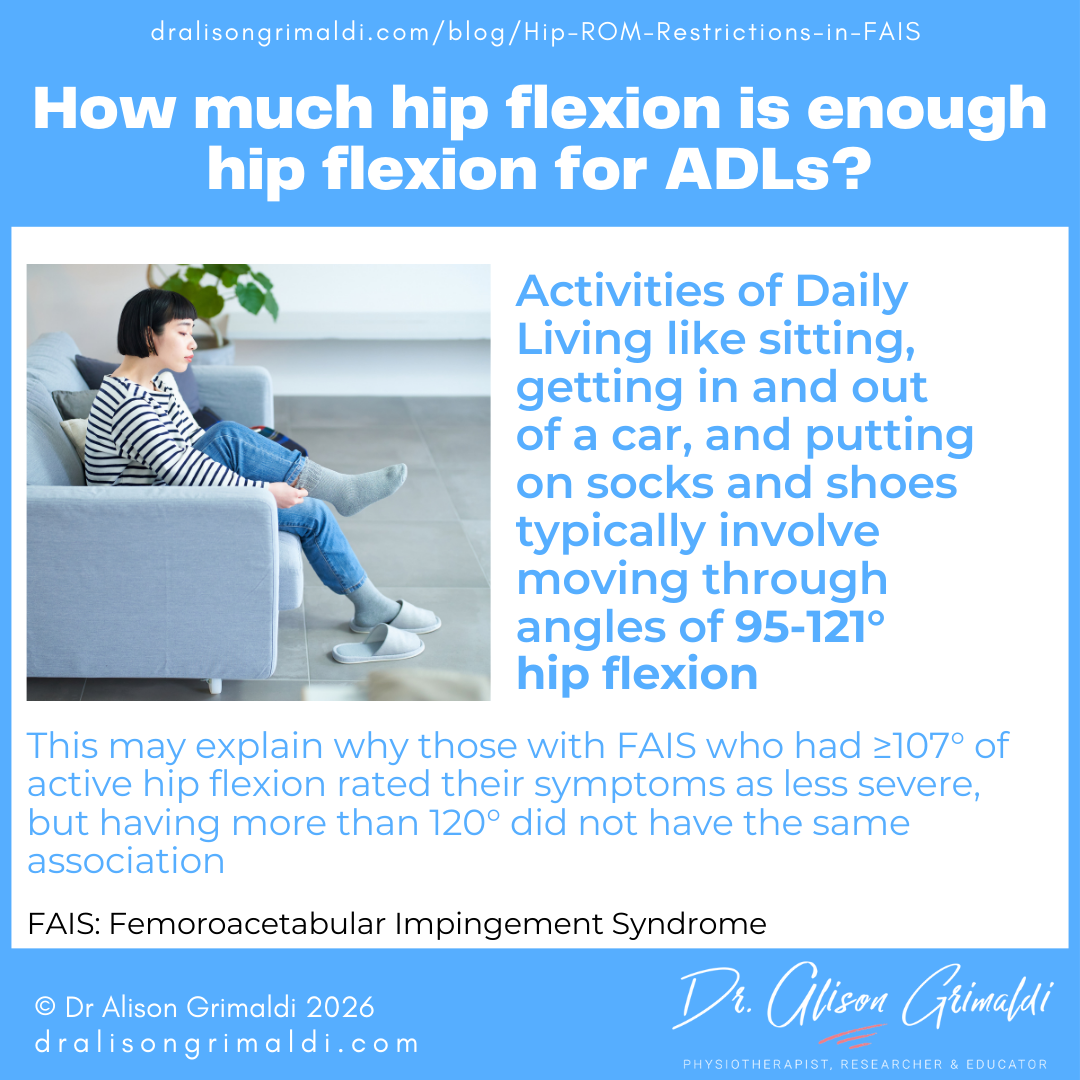
Adequate hip flexion range is important for key activities of daily living (ADLs), and many sports. ADLs like sitting, getting in and out of a car, and putting on socks and shoes typically involve moving through hip flexion angles of 95-121°.3,4
If you only have ≤107° of hip flexion range, and you experience pain with hip flexion, you are likely to score more poorly on the iHot symptom severity subscale (measuring pain, stiffness and functional limitations). If you have ≥120° of hip flexion, then you probably have enough for most ADLs, and the relationship drops away.


Want more? Gain access to all online hip courses, live and recorded masterclasses, Q & A sessions and Member Case sharing, and exclusive access to our entire how-to video library, ebook series and pdf resource library - diagnostic cheat sheets, condition info, management strategies & so much more.
Click here to find out how.
Hip flexion ROM may be important for optimal outcomes, for those with FAIS and <107◦
The data presented in the Gomes paper is only baseline data and the outcomes paper from the PhysioFirst trial has not yet been published. It is unclear yet how ROM at baseline, and changes in ROM over time may mediate outcomes of the treatment interventions of this trial. This will be interesting, as one intervention focused on strengthening and the other on stretching.2
Previous work by Jo Kemp and colleagues reported that active hip flexion ROM was the only ROM that was associated with 1-2-year outcomes of hip arthroscopic surgery for chondrolabral pathology (HOOS & i-HOT 33 scores).5 They suggested a threshold value of 100° of hip flexion, whereby hip flexion of >100° was linked with better post-surgical outcomes.
These studies have established that low hip flexion ROM is associated with worse FAIS symptoms and worse outcomes after hip arthroscopy. So, as the authors suggest, it stands to reason that patients with FAIS (and post-scope patients) may benefit from interventions that aim to increase hip flexion to at least 100°, and preferably between 107 and 120°.
However, if the patient has less than 107degrees of hip flexion, this DOES NOT mean that we should passively mobilise them and give them end-range flexion exercises, to increase their ROM and therefore their chances of success. STOP! And read on …
Match your treatment to the individual with FAIS. Considering the underlying reasons for range restrictions, may be CRITICAL to the outcomes of your treatment.


There is likely to be limited benefit in chasing hip rotation range in FAIS treatments
Considering the weak relationships between rotation range and symptoms, and lack of relationship between rotation range and outcomes after hip arthroscopy, spending time chasing rotation ROM may not be the best investment.
Gomes et al (2025) reported that an increase of 19° of hip internal rotation ROM would be needed to achieve a minimal clinically important change in the iHOT-symptoms score (8 points).1 That’s a lot! And previous work has shown that neither surgical nor physiotherapy interventions are terribly useful for increasing hip rotation ROM in those with FAIS.6-8
As for flexion ROM, how effectively we can increase hip ROM will depend on the underlying reasons for range limitations. These limiting factors will also influence your treatment approach.
Reasons for limited hip ROM in patients with FAIS and what to do about it
Before taking action, we MUST understand the factors that are most likely to be limiting hip ROM.
Bony impingement and range restriction in FAIS
The very definition of FAI is centred around range restriction related to early bony impingement of the femoral head-neck junction against the acetabular rim. Primary cam morphology (a bump at the head-neck junction) is one of the most common and impactful bony shapes that contributes to painful hip impingement (FAIS).
The Gomes study1 reported that cam morphology size did not alter the relationships between active hip ROM and symptom severity in patients with FAIS. However, it’s important to consider 2 things: i) the way ROM was measured and ii) that cam morphology is not the only structural limiter to ROM (think acetabular overcoverage and femoral retroversion).
When a patient moves their hip actively, a lack of available range will quickly be accommodated by shifting the motion to adjacent joints. In the Gomes study, the range measured was active ROM, and while the opposite thigh was strapped to the bed, this is inadequate to prevent pelvic motion. Other research has shown that sagittal plane hip motion without pelvic stabilisation is significantly different to ROM measured with the pelvis stabilised.9 And, that’s with passive ROM. Active ROM without pelvic stabilisation is likely to be poorly reflective of passive range restrictions associated with bony impingement.
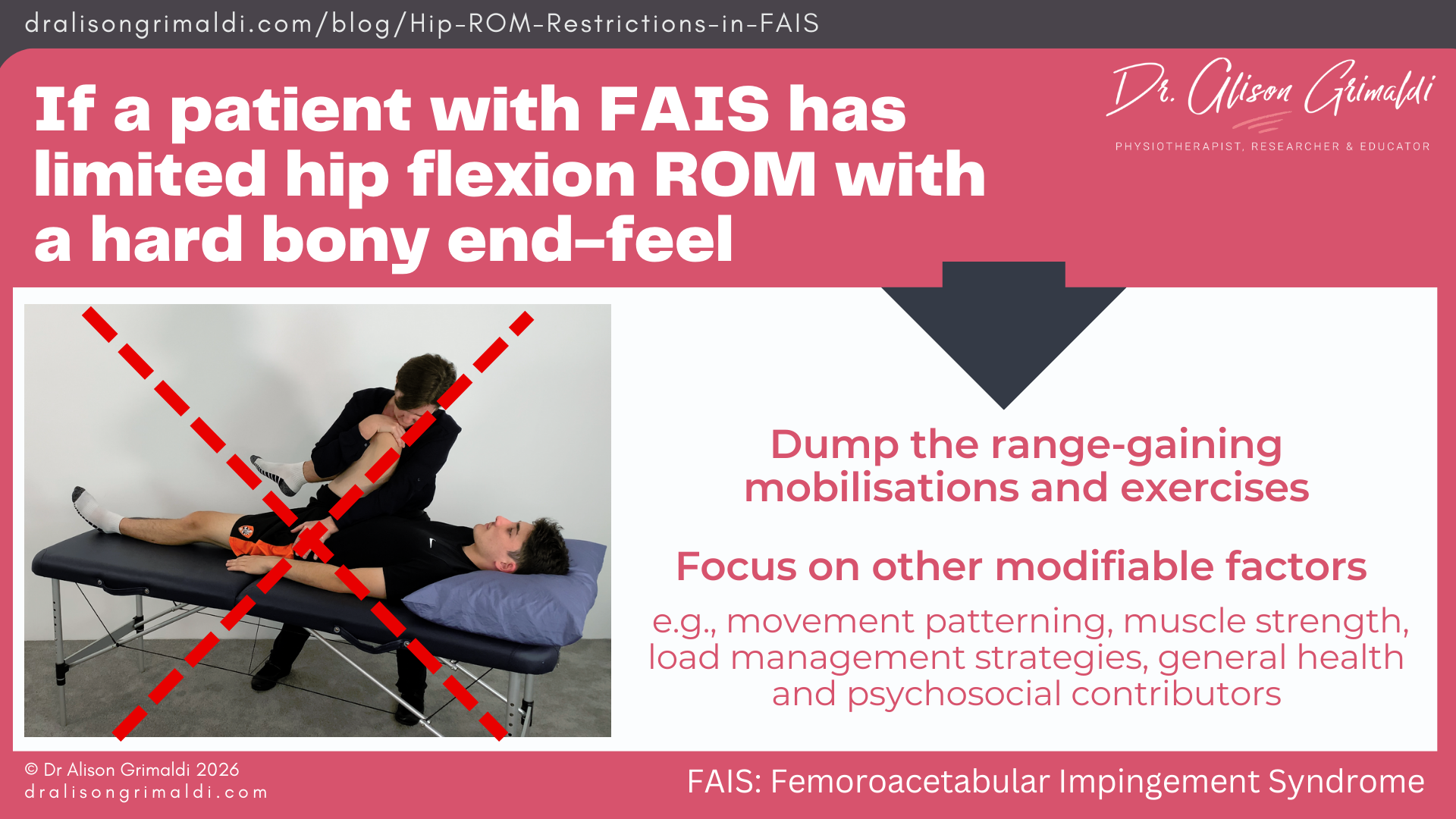
To try to tease out the potential contributing factors then, it’s important to also assess passive range of hip motion and end-feel. Either monitor when the pelvis first moves as you passively move the femur (a measure of relative flexibility) or stabilise the pelvis and assess the pure hip range.
What do you feel at the end of that passive hip range? Do you feel a hard bony block? In flexion, does the femur start deviating into abduction and external rotation (obligatory abduction-ER)? If the end feel is an early bony block, and especially if the ROM of hip flexion is less than 100°, there would be no sound rationale for passive range-gaining manual therapy techniques, or range-gaining exercises moving into end-range. Worst case scenario, you may make the patient considerably worse.
Actions:
Focus on the other modifiable factors would in this case be more appropriate – movement patterning, muscle strength, load management strategies and addressing any other modifiable general health and psychosocial contributors.
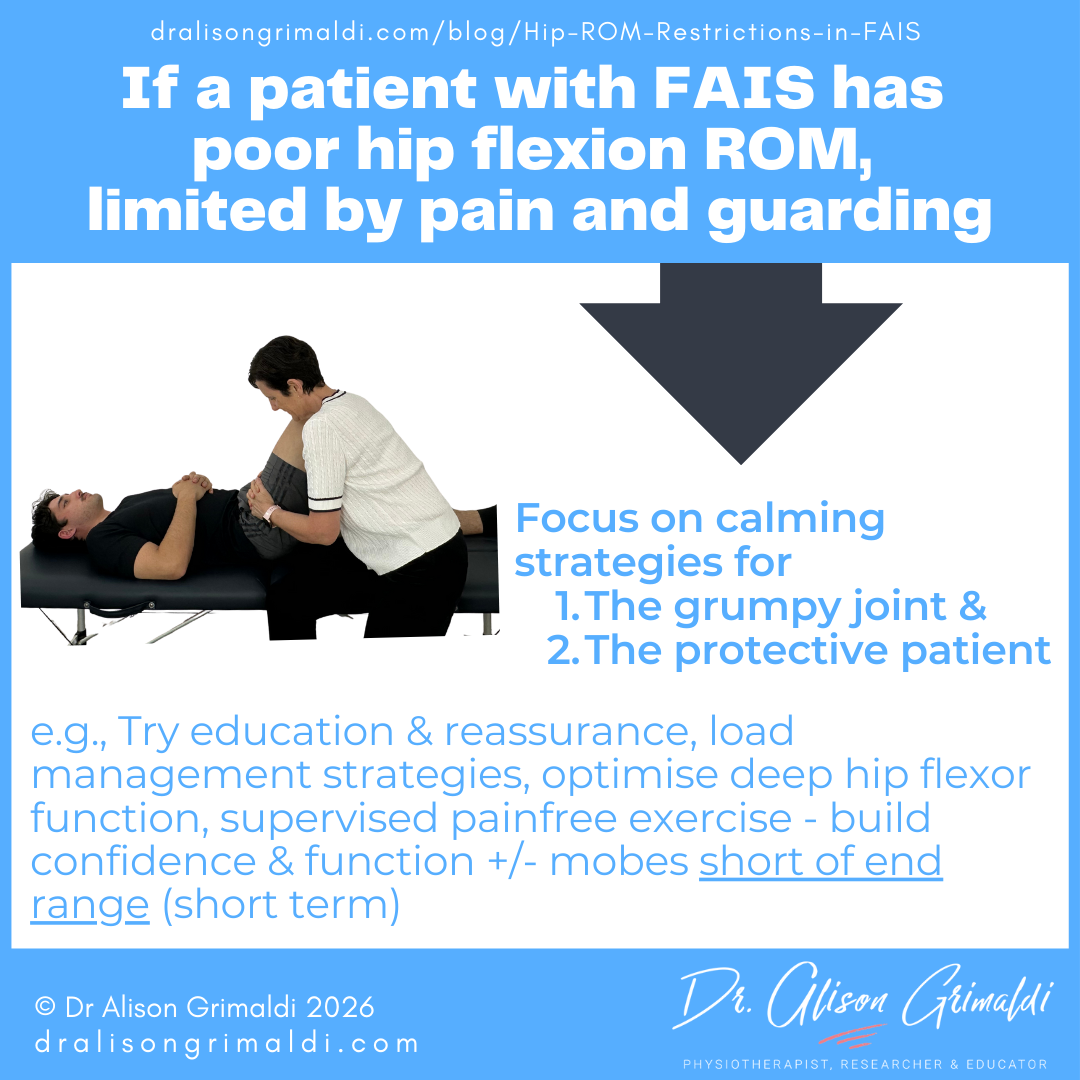
Grumpy hips and protective patients – ROM limitation related to pain, effusion and self-protection
Perhaps when you performed your passive movement assessment, you didn’t feel a hard bony block. In fact, it seemed like you got no-where near the true structural end-of range. All you felt was muscle guarding - a type of stuttery rigidity, preventing you from reaching what you might consider end-of-range.
This is the patient trying to protect themselves, either consciously or subconsciously. If there is significant intra-articular inflammation and effusion, the effusion itself may impact on ROM, but there is also often accompanied muscle guarding around the joint.
The guarding may also be related to pain or perceived threat of pain or damage to their hip. If the patient has already had a diagnosis of FAI, and done some internet scrolling about the topic, you can understand the response!
If their hip tends to be a bit ‘musical’ during active motion, this may also cause them to limit their hip motion. A recent qualitative paper of active adults with FAIS reported that those with hip crepitus (grinding, catching, or clicking in the hip) modify their activities, especially hip flexion movements, due to the sensation of hip crepitus.10
You may also note a guarding response from those with concurrent hip microinstability – yes, those with hip impingement can also have instability. Another good reason to let go of the ‘limited hips need mobilising’ mantra.
Actions
When you find hip ROM is limited by guarding:
- Reassess your technique
- Always test the non/least painful side first and explain to the patient exactly what you are doing.
- Ask the patient to let you know if they experience any pain – get a gauge of the level of pain and permission to move further if there is only mild discomfort.
- Provide more support to the moving limb, to ensure the patient feels adequately supported and able to relax.
- Some gentle manual therapy, short of pain and with good limb support may be helpful - more appropriate for the patient without instability.
- Get started on some active or active assisted exercise short of pain, with early focus on good control of deep hip musculature – most important for those with hip instability.
- Teach good load management strategies – this will be important to calm a ‘grumpy joint’, and reduce kinesiophobia and boost patient confidence in self-managing their condition.

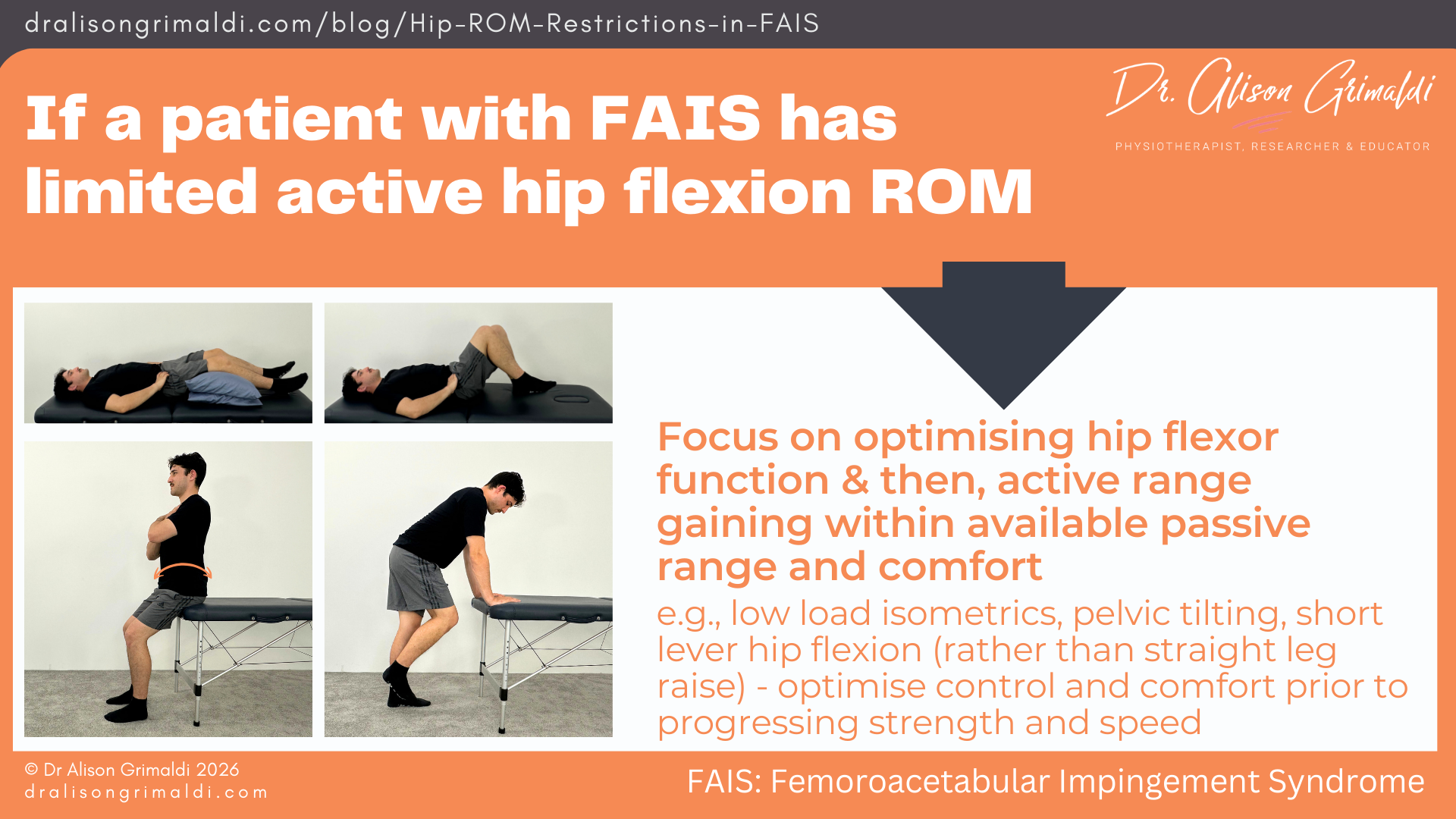
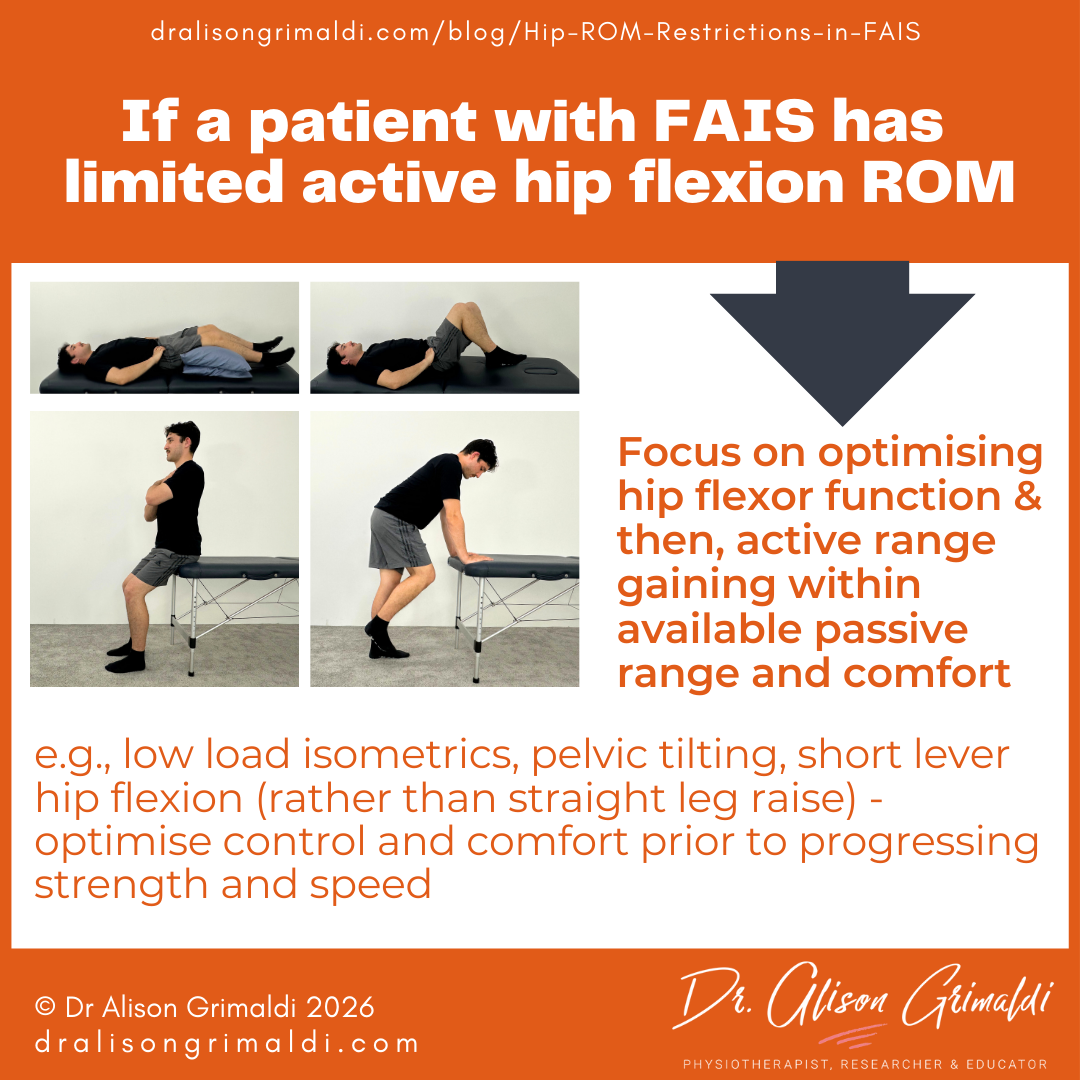
Limitation of active hip flexion range related to hip flexor dysfunction
One of the other main reasons for limitations in active range of motion, is muscle weakness or dysfunction in the members of the movement synergy required to move the hip joint into inner range – the deeper/uniarticular hip musculature.
Those with FAIS are generally weaker globally around their hip.11 Inner range deficits in active range of hip flexion may also reflect specific inhibition or dysfunction of the deep hip flexors – the iliopsoas and iliocapsularis. The iliopsoas muscle has the greatest physiological cross-sectional area within the hip flexor group and the overall best capacity to move the hip into ranges above 90degrees of hip flexion.
During ultrasound assessment of hip flexor function in clinic, we commonly see a loss of early recruitment of these deep hip flexors and reduced co-ordination of the hip flexor group in those with joint related hip pain. Such dysfunction is also often concurrent with pain and difficulty moving actively into inner range flexion.
If one of the key reasons for poor active range of hip flexion is hip flexor dysfunction, you’ll notice that the passive range of motion is usually notably greater than the active range achieved. Another good reason to assess both.
Actions
- Provide a graduated program of hip flexor exercises, focusing initially on good early recruitment of the deep hip flexors. Ultrasound biofeedback is fantastic for this, but palpation can also provide good guidance.
- Isometric and low-load hip flexor training can also be useful for situations where range is limited by fear or guarding. Optimised deep muscle recruitment may assist in supporting a joint with microinstability, alter direction of joint vectors and/or provide a reassuring feeling of control to the patient.
I hope this has provided some context around range restrictions in patients with FAIS, and other hip joint related conditions, and some ideas regarding appropriate actions depending on the examination findings.
If you’d like to learn more about assessment and management of FAIS and other hip conditions, come along to an upcoming live Anterior Hip & Groin Pain Workshop (F-2-F or online), take the Anterior Hip and Groin Pain online course, or join us in Hip Academy.

This blog was written by Dr Alison Grimaldi
Dr Alison Grimaldi is a physiotherapist, researcher and educator with over 30 years of clinical experience. She has completed a Bachelor of Physiotherapy, a Masters of Sports Physiotherapy and a PhD, with her doctorate topic in the hip region. Dr Grimaldi is Practice Principal of PhysioTec Physiotherapy in Brisbane and an Adjunct Senior Research Fellow at the University of Queensland. She runs a global Hip Academy and has presented over 100 workshops around the world.
References
- Gomes DA, Heerey J, Scholes M, et al. More is not always better-association between hip range of motion and symptom severity in patients with femoroacetabular impingement syndrome: A cross-sectional study. Braz J Phys Ther. 2025;29(2):101189.
- Kemp JL, Johnston RTR, Coburn SL, et al. Physiotherapist-led treatment for femoroacetabular impingement syndrome (the PhysioFIRST study): a protocol for a participant and assessor-blinded randomised controlled trial. BMJ Open. 2021;11(4):e041742. Published 2021 Apr 7.
- Han S, Kim RS, Harris JD, Noble PC. The envelope of active hip motion in different sporting, recreational, and daily-living activities: a systematic review. Gait Posture. 2019;71:227–233.
- Hyodo K, Masuda T, Aizawa J, Jinno T, Morita S. Hip, knee, and ankle kinematics during activities of daily living: a cross-sectional study. Braz J Phys Ther. 2017;21(3):159-166.
- Kemp JL, Makdissi M, Schache AG, Finch CF, Pritchard MG, Crossley KM. Is quality of life following hip arthroscopy in patients with chondrolabral pathology associated with impairments in hip strength or range of motion?. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3955-3961.
- Palmer AJR, Ayyar Gupta V, Fernquest S, et al. Arthroscopic hip surgery compared with physiotherapy and activity modification for the treatment of symptomatic femoroacetabular impingement: multicentre randomised controlled trial. BMJ. 2019;364:l185.
- Aoyama M, Ohnishi Y, Utsunomiya H, et al. A prospective, randomized, controlled trial comparing conservative treatment with trunk stabilization exercise to standard hip muscle exercise for treating femoroacetabular impingement: a pilot study. Clin J Sport. 2019;29(4):267–275.
- Emara K, Samir W, Motasem el H, Ghafar KA. Conservative treatment for mild femoroacetabular impingement. J Orthop Surg (Hong Kong). 2011;19(1):41–45.
- Beneck GJ, Selkowitz DM, Janzen DS, Malecha E, Tiemeyer BR. The influence of pelvic rotation on clinical measurements of hip flexion and extension range of motion across sex and age. Phys Ther Sport. 2018;30:1-7.
- Serighelli F, Snowdon DA, Barton CJ, et al. "I think there is something not right in my body": Beliefs and attitudes of active adults with hip/groin pain towards hip crepitus - A qualitative study. Musculoskelet Sci Pract. 2025;80:103427.
- Freke MD, Kemp J, Svege I, Risberg MA, Semciw A, Crossley KM. Physical impairments in symptomatic femoroacetabular impingement: a systematic review of the evidence. Br J Sports Med. 2016;50(19):1180.