6 of 12 Top Hip Papers of 2025 | Imaging findings from the LEAP gluteal tendinopathy clinical trial

It's Day 6 of my series of miniblogs featuring 12 top hip papers of 2025. Half way already!! Hope you've enjoyed the first 5. If you missed Day 5, you'll find a link at the bottom of this page to take you back. For day 6, I'm excited to share a secondary analysis from the LEAP trial that examined imaging findings in those with gluteal tendinopathy! Why is this exciting, you might think? Because I'm sure you field questions about imaging results reporting gluteal tendon tears all the time. This paper will provide some great insights into how common these are, in a population in which an education and exercise approach provided a circa 80% success rate. Read on to find out more.
(Half way through the 12 days of our Christmas special as well. Don't miss out!)
SPECIAL Xmas Offer!
Read until the end to claim a very special Christmas offer I have prepared just for you!
LIMITED TIME ONLY! ENDS MIDNIGHT 24th DECEMBER

6 of 12 Top Hip Papers of 2025: Imaging findings from the LEAP gluteal tendinopathy clinical trial1
Background:
In community health care, patients often receive news of tears in their gluteal tendons from imaging reports. This can invoke not only fear but assumptions that they will need a surgical repair. This paper will help you put things into a little more perspective for your patients, in an evidence based manner.
In this study, we examined the location, severity and clinical relevance of gluteal tendon pathology in the 204 participants of the LEAP clinical trial for gluteal tendinopathy.
The study was a prospective observational secondary analysis of data from a three-arm randomised clinical trial (RCT) involving 204 participants (167 females, mean age 54.8 years) with gluteal tendinopathy (GT) randomised to receive education-and-exercise, corticosteroid injection or a wait-and-see approach.
Study Aims:
- To examine the type and extent of imaging-detected changes in the tendons of gluteus medius (GMed) and gluteus minimus (GMin).
- To determine if the severity of trochanteric soft-tissue pathology rated on Magnetic Resonance Imaging (MRI) was associated with patient features of pain, function and disability.
What was done:
We performed a prospective observational secondary analysis of MRI and radiographic data from the LEAP RCT cohort, and investigated relationships between severity of pathology on MRI and pain, function and disability.

Method:
- MRI and x-ray images were evaluated by experienced radiologists, blind to clinical findings, who reported on location of tendon pathology, presence and severity of tendon tears and location and presence of calcification.
- Severity of changes seen on MRI were scored and analyses for relationships to pain, function and disability were performed.
Key Findings:
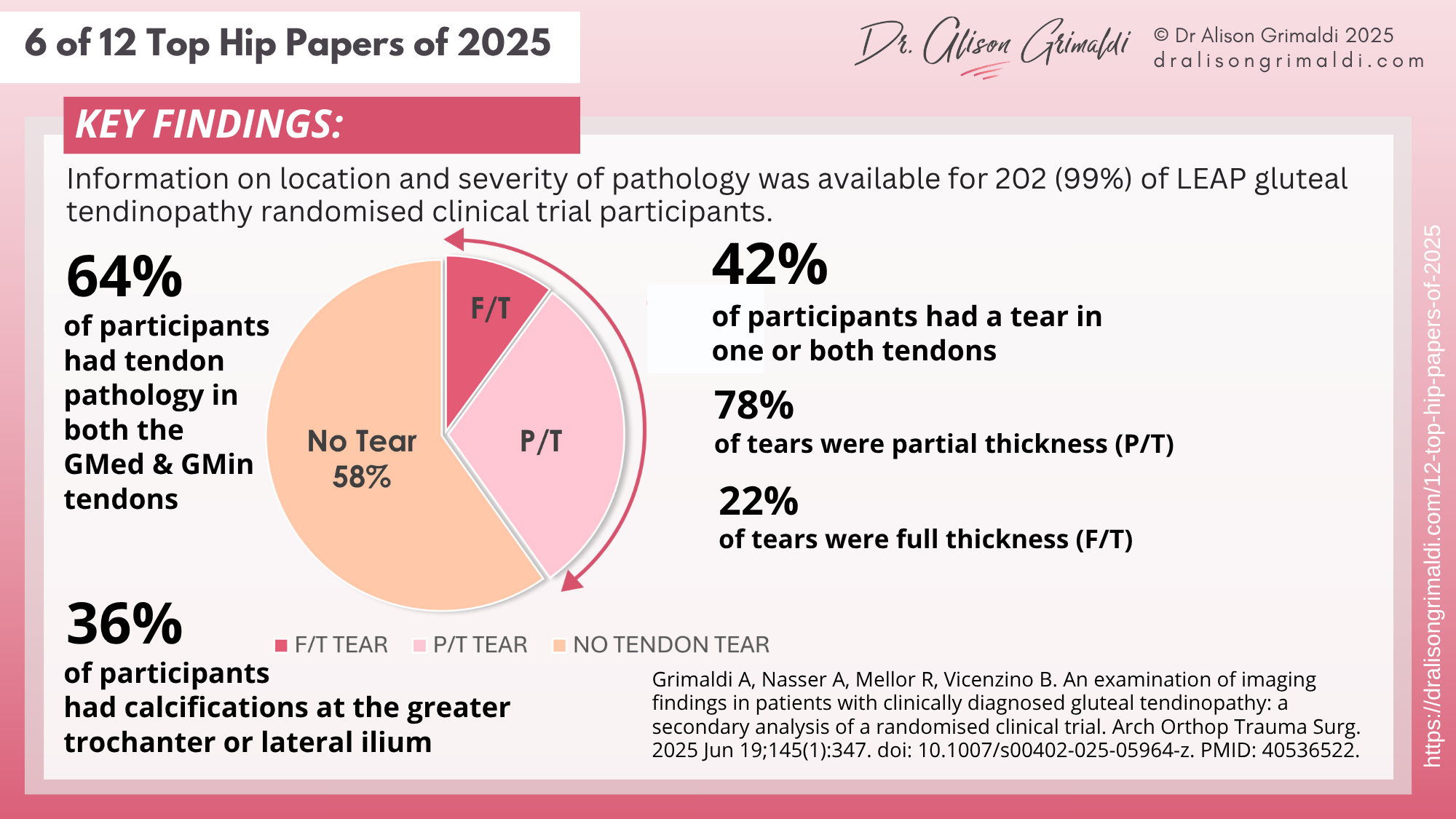
Gluteal tendon pathology was often in both tendons, and tears were common in participants of the LEAP RCT:
- 64% of participants had tendon pathology in both the gluteal medius and minimus tendons
- 42% of participants had a tear in one or both tendons
- 78% of tears were partial thickness and 22% were full thickness.
Around 1 in 3 participants also had calcifications evident in the location of the tendons of insertion and/or origin of the trochanteric abductors
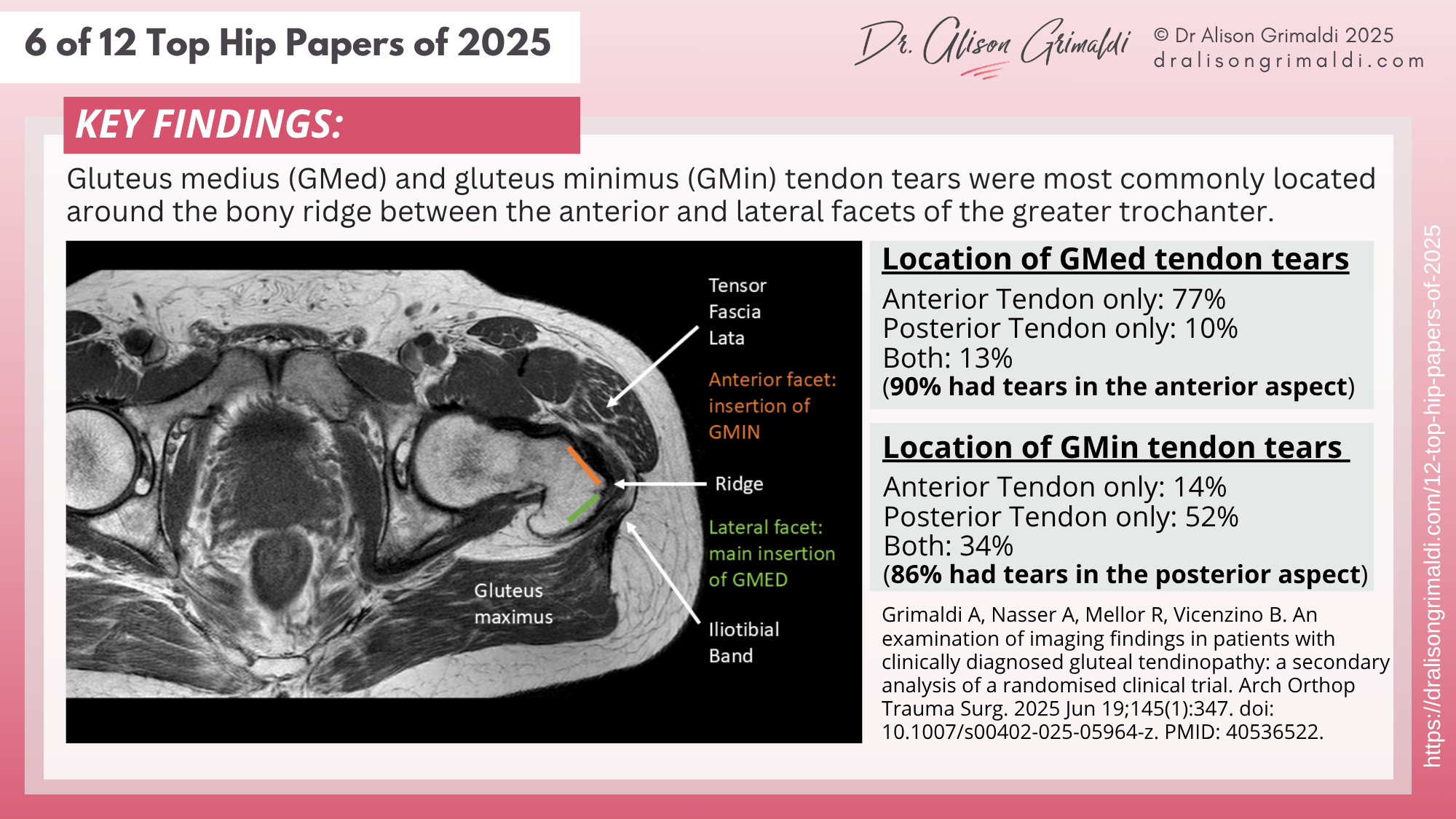
The location of gluteal tendon tears was also of interest:
- Gluteus medius tendon tears were much more likely to occur in the anterior portion of the tendon ( 77% occurred anteriorly, 10% posteriorly and 13% in both locations) - 90% had tears in the anterior aspect of the GMed tendon.
- Gluteus minimus tendon tears were much more likely to occur in the posterior portion of the tendon (only 14% occurred anteriorly, 52% posteriorly and 34% in both locations) - 86% had tears in the posterior aspect of the GMin tendon.
This is interesting because the worst pathology appears to be focused around the apex of the greater trochanter - the ridge where the anterior and lateral facets meet. This area may be exposed to high levels of compression from the overlying iliotibial band. Load management advice and movement training to reduce adduction and compression from the overlying ITB will be important to reduce compression over the bony ridge.
Pain, function and disability of people with gluteal tendinopathy were not associated with the severity of tendon changes on MRI, in participants of the LEAP clinical trial.
Clinical Implications:
Gluteal tendon tears were common in participants of the LEAP RCT, BUT
- the severity of pathology was not clinically relevant in this group.
- tendon tears were present in 49% of those who undertook the education and exercise intervention, which returned a 77–78% success rate and superiority over other interventions (CSI and wait-and-see) in terms of patient-reported global improvement at 8 and 52 weeks.
- a previously published moderator analysis revealed that the severity of tendon pathology in the LEAP cohort did not significantly influence the difference in outcomes between treatments.
Education-and-Exercise is an appropriate and recommended first-line treatment for gluteal tendinopathy, regardless of the presence of partial or full thickness tendon tears or calcifications
We found that, despite previous assumptions made about our cohort, participants of the LEAP RCT commonly had pathology in both the GMed and GMin tendons, with tendon tears present in one or both tendons in 42%, and calcifications were visible on x-ray in 36%.
Why is this important?
- Often patients and health professionals reading a finding of a gluteal tendon tear on an imaging report will assume that some form of medical intervention may be required - for example an injection or surgery.
- Previously published 'staged treatment guidelines' recommended such an approach, having made assumptions about the LEAP trial cohort (that our participants had no tears).
- The LEAP Education and Exercise management approach provided a near 80% success rate in both the short and long term, despite high prevalance of partial and full thickness tendon tears (49% of this group had tears in one or both tendons).
- We also showed severity of clinical presentation was not linked with severity of tendon pathology in the LEAP cohort, and our previous work showed it did not mediate outcomes.
Our findings contribute to the evidence base that suggests:
Education-and-Exercise is an appropriate and recommended first-line treatment for gluteal tendinopathy, regardless of the presence of partial or full thickness tendon tears or calcifications.

SPECIAL HOLIDAY OFFER!
$100 OFF
your Hip Academy joining fee
Offer Only Available During the 12 Hip Days of Christmas (13th-24th December). Do not miss this exclusive offer!
Now only AUD $345 (usually $445) to join to receive immediate access to over $4,800 worth of content!!
(AUD$345 equates to approximately 181 GBP and 230 USD)
USE COUPON CODE: xmas25hip
Like to learn more about managing gluteal tendinopathy?
In this course, you can find detailed information on pathoaetiology, assessment and management of lateral hip pain associated with gluteal tendinopathy (greater trochanteric pain syndrome, trochanteric 'bursitis'), and many other conditions. To learn more, take the online course, or join me in a workshop.
This online course is included in Hip Academy and Hip Academy members receive discounts for online workshops.