Greater trochanteric pain after hip replacement

Are you struggling to confidently diagnose and treat lateral hip pain in your patients?
Many surgeons consider trochanteric pain a relatively minor complication following arthroplasty, however the impact can be substantial, with significant reductions in post-operative satisfaction, quality-of-life and functional outcomes.1,2,3 Those with greater trochanteric pain have been reported to have quality-of-life and levels of disability similar to those with advanced hip osteoarthritis.4 Therefore, the benefits of alleviation of joint pain by arthroplasty may not be realised by many patients who experience abductor pain and dysfunction after hip replacement surgery.
Corticosteriod injection for trochanteric pain after hip replacement is a common treatment, but has accompanying risks and should not be first-line management. Better understanding of why trochanteric pain occurs after total hip replacement is key to developing more appropriate treatment approaches and prevention strategies.
Abductor dysfunction in the form of weakness and functional deficits such as a Trendelenburg gait may also persist or worsen after hip arthroplasty. This may be related to trochanteric pain or to neurological injury or mechanical impairment associated with the surgical technique. Even in the absence of hip pain, a significant gait disturbance associated with iatrogenic hip abductor muscle impairments may result in a longer-term reliance on walking aides. Pain may also develop in adjacent regions, most commonly the lumbar spine or knee, due to the hip abductor muscle dysfunction, altered kinematics and loads transferred to these regions.
Abductor pain following hip replacement surgery, or total hip arthroplasty has been reported with varying incidence, as low at 1.7%,5 but as high as 29% in a broad population.3 The incidence of trochanteric pain has been reported to be even greater in young (49.9 ± 7.1 years), active patients - 37% after total hip arthroplasty and 35% after resurfacing.6 The development of greater trochanteric pain after hip replacement surgery is also more likely to occur in females.2
If a patient presents to your clinic with abductor pain and dysfunction after hip replacement surgery, there are usually 3 main scenarios:
- They had co-morbid gluteal tendinopathy prior to hip arthroplasty – recognised or unrecognised.
- They had pre-clinical gluteal tendinopathy pre-operatively that became symptomatic post-operatively.
- The abductor mechanism was adversely impacted by the surgery, resulting in abductor pain and/or dysfunction.
Persistent lateral hip pain after hip replacement, associated with gluteal tendinopathy
Pain associated with hip osteoarthritis is most commonly experienced deep in the mid-inguinal region anteriorly, around the anterolateral hip (c-sign) or deep at the front, back and side of the hip (triangulation sign), together with various areas of referral to the thigh, knee and anterolateral shin. Pain in the greater trochanteric region is also common (57% - 77%) in those with hip osteoarthritis.7,8 This trochanteric pain can be associated with direct referral from the hip joint, or co-morbid gluteal tendinopathy, or both. Gluteal tendon tears have been reported to be present in 20% of patients undergoing total hip arthroplasty,9 with the prevalence of gluteal tendinopathy with or without tear likely to be much higher. In those with hip osteoarthritis, concurrent tendinopathy may be detected pre-operatively and addressed within the constraints of the osteoarthritic joint. However, for many patients the additional diagnosis is missed prior to arthroplasty, the trochanteric pain assumed to be related to the joint pathology. Following surgery then, while much of their pre-operative hip pain will be relieved, the trochanteric pain may persist.
What can clinicians do to reduce persistent lateral hip pain after total hip replacement?
Approach to gluteal tendinopathy pre-operatively & throughout the OA journey:
- Ensure any pre-operative gluteal tendinopathy is identified (don’t just assume all the pain is related to the osteoarthritis)
- Identify and address any aberrant loading patterns that may be impacting on the gluteal tendons – education, load management, movement training, aides as required
- Address abductor disuse associated with habitual unloading in weightbearing – standing, squatting, sit-stand, gait
- Address specific dysfunction in the abductor synergy – the deeper and anterior portions of the gluteus medius and minimus are usually most prone to atrophy
- Maintain abductor muscle strength as much as possible within the confines of the joint pain
Approach to gluteal tendinopathy after total hip replacement:
- Start low-load isometric abductor loading from day 1
- Optimise movement patterns and recruitment of the abductor muscles
- Graduate abductor exercise and return to activity, allowing time for the tendons to adapt
- Educate the patient about managing the persistent tendon condition
- Monitor response to exercise and adjust as required
Development of lateral hip pain after hip replacement, associated with pre-clinical gluteal tendinopathy
For others, trochanteric pain may have never been a major feature of their hip osteoarthritis presentation, but they may develop lateral hip pain following hip replacement. This can be related to pre-existing but asymptomatic pathology of the gluteal tendons. The pain is usually not evident immediately after surgery but develops over a period of weeks or months. One study reported that 82.4% (472/573) of their participants with greater trochanteric pain following hip arthroplasty were diagnosed at greater than 6 months postoperatively.5 This doesn’t necessarily mean that pain onset was after 6 months, but that the diagnosis was reached at that point. Hip pain in the first few months following total hip replacement is usually assumed to be related to healing bone and soft tissues. After 6-months, the tissues impacted by the surgery should have healed adequately, so if radiographs obtained indicate no bony issues and a well-situated prosthesis, persistent pain may be attributed to other soft tissue conditions such as gluteal tendinopathy.
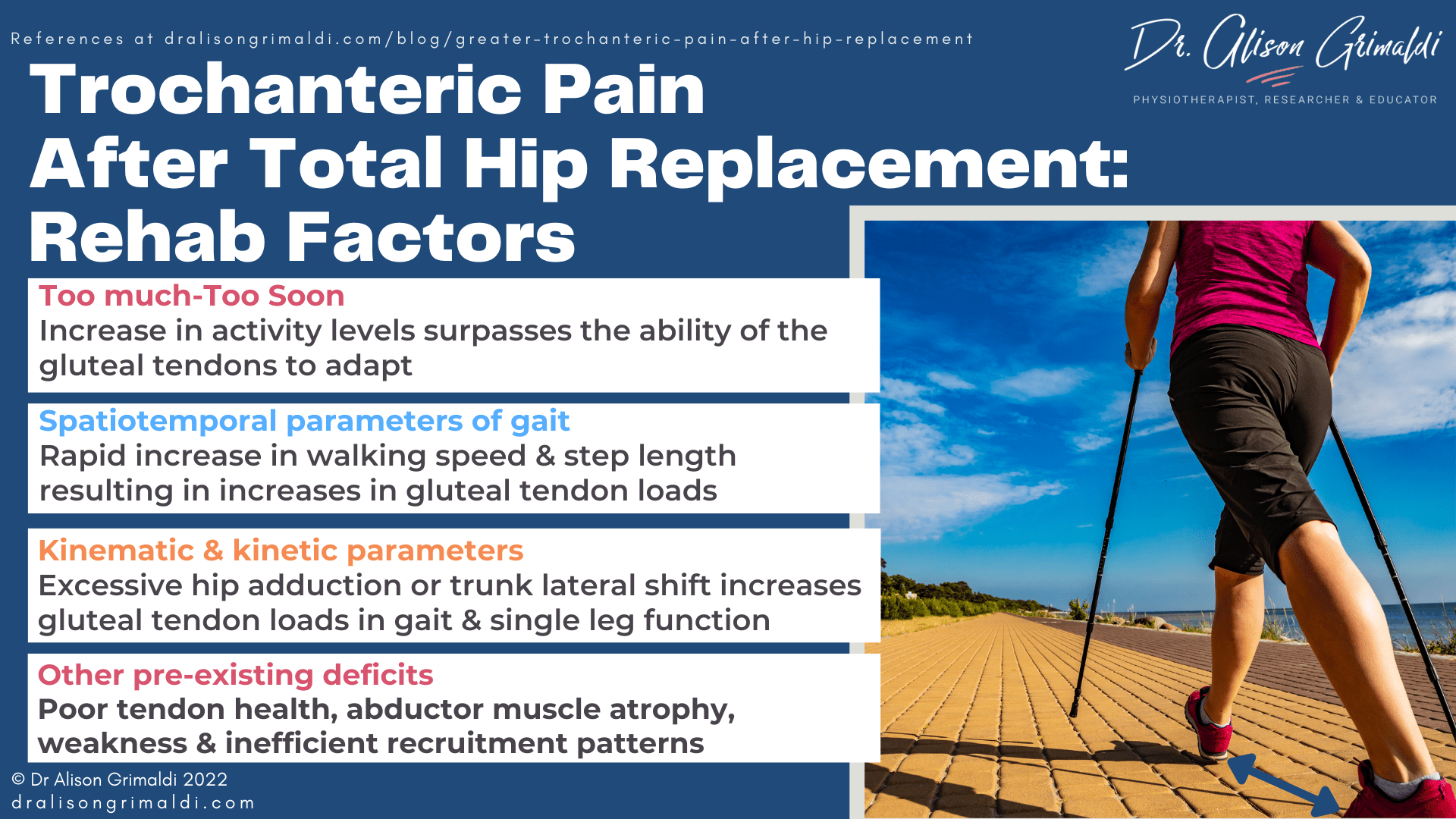
Onset of lateral hip pain following total hip replacement often occurs between 6 and 12 weeks post operatively. This is usually when the patient recovers adequately from the arthroplasty to start walking longer distances and at greater speeds. Spatiotemporal parameters of gait have been shown to significantly improve within 6 weeks of total hip arthroplasty.10 Participants in this study were walking at faster speed and with greater step length than pre-operatively and although speed was still not comparable to healthy individuals even at 12 months, step length was comparable by 6 weeks.10
Gait speed and step length can both influence the external hip adduction moment, and the corresponding internal hip abduction moment – load on the abductor mechanism (Allison). The hip abductor tendons have usually been relatively underloaded during the later stages of hip osteoarthritis, due to reduced activity levels and specific unloading of the painful side during standing and functional tasks. As activity levels and walking speed and step length increase post operatively, if the increase in load surpasses the ability of the tendon to adapt, trochanteric pain may develop. The presence of gluteal tendon pathology will reduce the ability of the tendon to adequately adapt. Often on questioning, the patient may have had a history of episodes of lateral hip pain in the earlier stages of their hip osteoarthritis, but in the later stages with reduced activity and load this may not have settled or been eclipsed by other more severe joint related pain.
Surgical impact on the abductor mechanism resulting in abductor pain and dysfunction following hip replacement surgery
The other main scenario explaining abductor pain following total hip replacement surgery, is one in which the surgery itself has resulted in inadvertent damage, or a change in abductor loads. There may also be a surgical impact on abductor muscle function, with or without abductor pain.
Impact of surgical technique on the abductor tendons or abductor muscle function
The direct lateral approach involves a direct insult to the gluteal tendons as they are detached to gain access to the joint and reattached once the prosthesis is in situ. This direct impact to the abductor tendons may result in pain inhibition of the gluteus medius and minimus and often the surgeon instructs a complete lack of any abductor exercises for 6 weeks. Abductor weakness may result. Poorer improvement in the abductor muscle strength at 12 months has been reported after a lateral approach compared with a posterior approach arthroplasty.12
Although the direct lateral approach might be expected to be most likely to result in abductor pain due to the surgical disturbance of these tendons, a recent study reported that the direct anterior approach demonstrated the highest risk and the direct lateral demonstrated the lowest risk for lateral trochanteric pain.5 The reason for the higher risk in the direct anterior approach was unclear – perhaps associated with the impact on the Tensor Fascia Lata or due to factors that were not directly related to surgical approach.
The relationship between posterior approach arthroplasty and post-operative trochanteric pain may be related to surgical damage to the gluteals or a change in tendon loads associated with positioning of the femoral stem and acetabular cup. The positioning of these components, and specifically the lateral offset of the femur, directly impacts abductor lever arm, abductor strength and soft tissue tension at the greater trochanter. Global offset of the femur is a combination of femoral offset and cup offset. The femoral offset is the distance between the centre of rotation of the head of the femur and the long axis of the femur. The cup offset is the distance between the centre of the head of the femur and a perpendicular line passing through the medial edge of the ipsilateral acetabular teardrop.13 Surgeons using a posterior approach are more likely to increase the femoral offset to increase hip stability due to soft tissue tension.14 While an increased femoral offset positively impacts on abductor lever arm and strength, the additional compressive load at the greater trochanter could contribute to the development of trochanteric pain associated with gluteal tendinopathy.
Inadequate offset in any approach may lead to abductor dysfunction and gait disturbance due to the disruption of the natural lever arm – the musculotendinous complex is now too long for the lever, resulting in a Trendelenburg type gait and difficulty actively contracting into inner range abduction. Mahmood and colleagues reported that a reduction in global femoral offset of more than 5 mm after total hip arthroplasty has an adverse impact on abductor muscle strength and should therefore be avoided.13
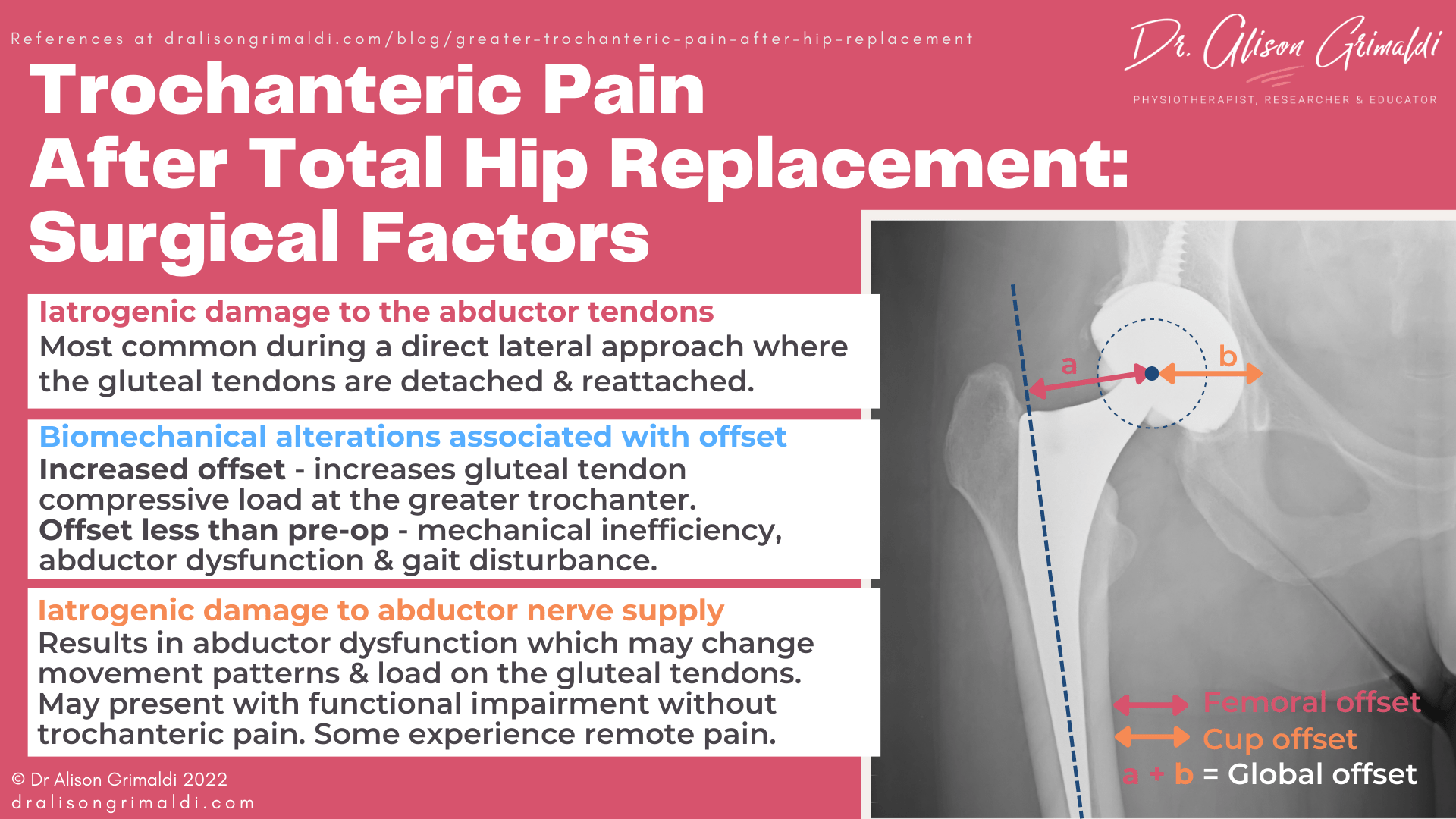
While the biomechanical relationship between global femoral offset and abductor muscle function appears fairly straight forward and consistent across studies, no significant correlations have been demonstrated between greater trochanteric pain and biomechanical factors such as femoral offset and leg length discrepancy following arthroplasty.1,2,15 It is possible that biomechanical factors associated with the prosthesis may still be a contributor to the development of trochanteric pain in some individuals, however there are likely to be other more important factors related either to direct surgical impact on the tendons depending on approach or most commonly, alterations in tendon loads related to changes in activity and spatiotemporal parameters of gait following surgery. Pre-existing poor abductor musculotendinous health and movement patterns are also likely to predispose to development of post-operative trochanteric pain related to surgical technique.
Gluteal nerve injury during total hip arthroplasty
You may also have treated patients after total hip arthroplasty who present with a substantial Trendelenburg sign early post-operatively, that just doesn’t seem to resolve in that first few months of rehabilitation. No matter what you do or how compliant your patient is, you just don’t seem to be able to significantly change abductor strength or that gait pattern. That may well be out of your control. If your patient has quite profound abductor weakness and gait disturbance, start suspecting a nerve injury.
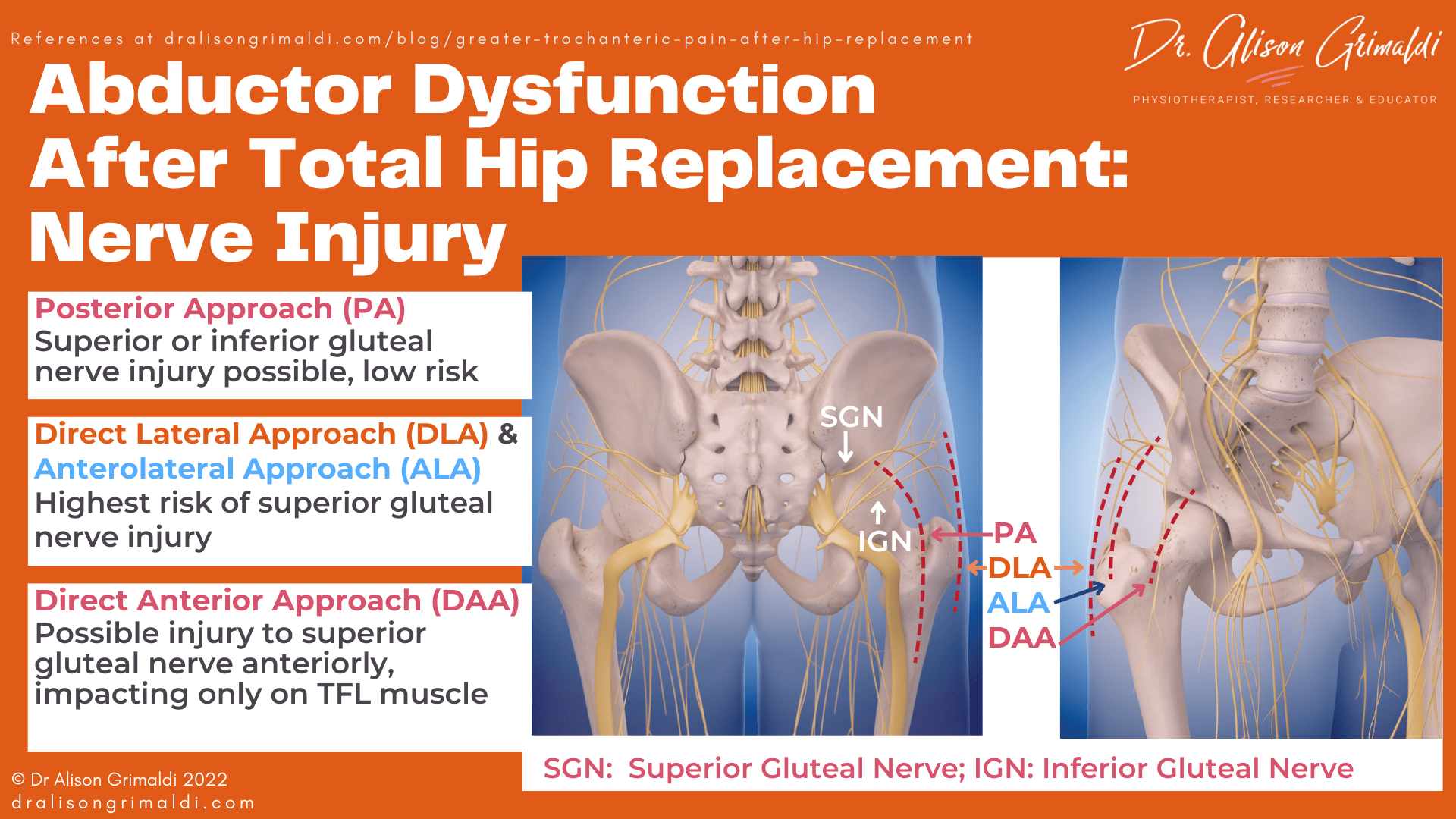
Abductor dysfunction following hip arthroplasty is sometimes the result of iatrogenic interruption to the nerve supply to the hip abductor muscles – the superior gluteal nerve. Your level of suspicion will vary depending on surgical approach. A posterior approach may result in injury to the superior gluteal nerve or the inferior gluteal nerve that serves the gluteus maximus, but the rates of this type of nerve injury during a posterior approach have been reported to be low.16
Iatrogenic superior gluteal nerve injury is most common during a direct lateral or anterolateral approach total hip arthroplasty, with up to 77% of all patients undergoing this approach having abnormal post-operative EMG findings related to some level of injury to the superior gluteal nerve.16 Most of these are categorised as ‘subclinical,’ but it’s possible that these subtle impacts on nerve supply may impact on motor control and response to standard rehabilitation. More severe injury results in a palsy of the hip abductors which results in a Trendelenburg sign and gross abductor weakness, impacting on gait patterns and single leg weightbearing function. These effects are reported to be largely temporary, with EMG returning to normal in almost all cases within 6 months.
Superior gluteal nerve injury may also occur in a direct anterior approach, where the most anterior branches of this nerve provide muscular supply to the Tensor Fascia Lata (TFL) muscle. Injury may be related to the incision, placement of retractors or impact on the blood supply (the ascending branch of the lateral circumflex femoral artery).17 This anterior injury only affects the TFL, therefore the impact on abductor function would not be as profound as a more lateral injury to the nerve prior to supply of the gluteus medius, minimus and TFL, most common in the direct lateral approach.
What can non-surgical healthcare professionals do about superior gluteal nerve injury after total hip arthroplasty?
- Understand that recovery occurs in most cases, but will often take 6-12 months
- Educate and reassure the patient
- Preserve the available abductor muscle function through exercise
- Consider direct electrical muscle stimulation in the case of palsy (always check with the surgeon, less useful for deeper muscle segments)
- Use walking aides as required to avoid abnormal loads on the prosthesis, lumbar spine and lower kinetic chain.
Abductor pain and dysfunction following hip replacement surgery are among the most common post-operative complications. While the surgeon may understandably be relatively unconcerned if the prosthesis is well placed and not the source of the issue, greater trochanteric pain can delay and reduce outcomes following total hip arthroplasty. In this blog, we’ve walked through the 3 main scenarios, the reasons why some patients develop or experience persistent lateral hip pain following arthroplasty. With an understanding of the why, clinicians involved in rehabilitation can identify and address gluteal tendinopathy in those with osteoarthritis and manage loading and return to activity following surgery. An important role of the non-surgical healthcare practitioner is to care for the soft tissues adjacent the prosthesis, to optimise outcomes of a potentially life-changing surgery for our patients.
If you are keen to hear more about prehabilitation & rehabilitation considerations for hip arthroplasty, we covered this topic in a Hip Academy meeting this year. All members can access recordings of previous lectures/meetings. Join up to catch up on some of the great topics we've covered.
HIP ACADEMY MEETING TOPIC:
Prehab & Rehab for Hip Arthroplasty
-
- the importance of rehab in the later stages of OA/prehab prior to arthroplasty
- key things we aim to maintain prior to surgery & strategies to achieve these
- how type of surgical approach influences your post-operative management
- precautions and priorities through different phases
References
- Bateman D, Wang M, Mennona S, Kayiaros S. Incidence of and Risk Factors for Lateral Trochanteric Pain After Direct Anterior Approach Total Hip Arthroplasty. Orthopedics. 2022 Mar-Apr;45(2):e79-e85.
- Iorio R, Healy WL, Warren PD, Appleby D. Lateral trochanteric pain following primary total hip arthroplasty. J Arthroplasty. 2006 Feb;21(2):233-6.
- Moerenhout K, Benoit B, Gaspard HS, Rouleau DM, Laflamme GY. Greater trochanteric pain after primary total hip replacement, comparing the anterior and posterior approach: A secondary analysis of a randomized trial. Orthop Traumatol Surg Res. 2021 Dec;107(8):102709.
- Fearon AM, Cook JL, Scarvell JM, et al. Greater trochanteric pain syndrome negatively affects work, physical activity and quality of life: a case control study. J Arthroplasty. 2014;29(2):383–6.
- Skibicki HE, Brustein JA, Orozco FR, Ponzio DY, Post ZD, Ong AC. Lateral Trochanteric Pain Following Primary Total Hip Arthroplasty: Incidence and Success of Nonoperative Treatment. J Arthroplasty. 2021 Jan;36(1):193-199.
- Nam D, Nunley RM, Sauber TJ, Johnson SR, Brooks PJ, Barrack RL. Incidence and Location of Pain in Young, Active Patients Following Hip Arthroplasty. J Arthroplasty. 2015 Nov;30(11):1971-5.
- Everett BP, Sherrill G, Nakonezny PA, Wells JE. The relationship between patient-reported outcomes and preoperative pain characteristics in patients who underwent total hip arthroplasty. Bone Jt Open. 2022;3(4):332-339.
- Poulsen E, Overgaard S, Vestergaard JT, Christensen HW, Hartvigsen J. Pain distribution in primary care patients with hip osteoarthritis. Fam Pract. 2016;33(6):601–606.
- Howell GE, Biggs RE, Bourne RB. Prevalence of abductor mechanism tears of the hips in patients with osteoarthritis. J Arthroplasty. 2001; 16(1):121-123.
- Bahl JS, Nelson MJ, Taylor M, Solomon LB, Arnold JB, Thewlis D. Biomechanical changes and recovery of gait function after total hip arthroplasty for osteoarthritis: a systematic review and meta-analysis. Osteoarthritis Cartilage. 2018 Jul;26(7):847-863.
- Allison K, Wrigley TV, Vicenzino B, Bennell KL, Grimaldi A, Hodges PW. Kinematics and kinetics during walking in individuals with gluteal tendinopathy. Clin Biomech (Bristol, Avon). 2016 Feb;32:56-63.
- Rosenlund S, Broeng L, Overgaard S, Jensen C, Holsgaard-Larsen A. The efficacy of modified direct lateral versus posterior approach on gait function and hip muscle strength after primary total hip arthroplasty at 12months follow-up. An explorative randomised controlled trial. Clinical biomechanics. 2016; 39:91-9.
- Mahmood SS, Mukka SS, Crnalic S, Wretenberg P, Sayed-Noor AS. Association between changes in global femoral offset after total hip arthroplasty and function, quality of life, and abductor muscle strength. A prospective cohort study of 222 patients. Acta Orthop. 2016 Feb;87(1):36-41.
- Kruse C, Rosenlund S, Broeng L, Overgaard S. Radiographic cup position following posterior and lateral approach to total hip arthroplasty. An explorative randomized controlled trial. PLoS One. 2018 Jan 29;13(1):e0191401.
- Abdulkarim A, Keegan C, Bajwa R, Sheehan E. Lateral trochanteric pain following total hip arthroplasty: radiographic assessment of altered biomechanics as a potential aetiology. Ir J Med Sci. 2018 Aug;187(3):663-668.
- Hasija R, Kelly JJ, Shah NV, Newman JM, Chan JJ, Robinson J, Maheshwari AV. Nerve injuries associated with total hip arthroplasty. J Clin Orthop Trauma. 2018 Jan-Mar;9(1):81-86.
- Grob K, Manestar M, Ackland T, Filgueira L, Kuster MS. Potential Risk to the Superior Gluteal Nerve During the Anterior Approach to the Hip Joint: An Anatomical Study. J Bone Joint Surg Am. 2015 Sep 2;97(17):1426-31.
Another great Lateral Hip Pain blog
Lateral Hip Pain: Causes, Diagnosis, and Treatment